Diabetic ketoacidosis – treatment and prevention

Diabetic ketoacidosis is the most common acute emergency in people with type 1 diabetes mellitus, and can be life-threatening. Education to improve early recognition and appropriate management may avoid the need for presentation to the emergency department and reduce morbidity and mortality.
- Diabetic ketoacidosis (DKA) is a life-threatening emergency that requires prompt treatment. The initial management of DKA involves fluid resuscitation and insulin administration.
- On diagnosing DKA in an outpatient setting, subcutaneous rapid-acting insulin should be administered immediately rather than waiting for the person to present to the emergency department. Antiemetics should be administered, if appropriate.
- Sodium-glucose cotransporter-2 inhibitors should not be prescribed by GPs for people with type 1 diabetes as there is a significantly increased risk of DKA. Off-label use and use for cardiac or renal indications in people with type 1 diabetes should only occur in carefully selected individuals under the close supervision and monitoring of a specialist endocrinologist.
- Insulin pump and infusion set (tubing, cannula) issues are the most common precipitant of DKA in people with type 1 diabetes using insulin pumps. If a person with type 1 diabetes using pump therapy unexpectedly develops ketosis, they should administer a subcutaneous dose of rapid-acting insulin via injection (dose calculated from the pump) and change their pump reservoir and infusion set.
Diabetic ketoacidosis (DKA) occurs when there is significant insulin deficiency that prevents the uptake of glucose by cells as an energy source.1 The body adapts by metabolising fats to generate ketones as an alternative source of energy. The production of ketones is acidic, resulting in ketoacidosis. Insulin deficiency typically results in concurrent hyperglycaemia.
Case scenario
Michael is a 22-year-old man who presents to you complaining of excessive fatigue, nausea, vomiting, abdominal pain, polyuria, polydipsia and blurred vision. He reports no recent infections. His past medical history includes type 1 diabetes mellitus, which was diagnosed when he was 19 years of age. He discloses that he ran out of his usual insulin two days ago (long-acting insulin 30 units at night and rapid-acting insulin 10 units three times daily with meals; total daily dose = 60 units).
On examination, he is pale, diaphoretic and drowsy with a Glasgow Coma Scale score of 14. He has normal blood pressure (103/72 mmHg) and body temperature (37.2°C) but is tachycardic (heart rate, 127 beats per minute) with cool peripheries and sluggish capillary refill. He is tachypnoeic (respiratory rate, 34 breaths per minute) with deep and rapid respiration (Kussmaul breathing) and accessory muscle use. His abdomen is soft but generally tender. His blood glucose level is elevated at 19 mmol/L with large urine ketones detectable and elevated blood ketones higher than 5 mmol/L (reference range <0.6).
You confirm a diagnosis of DKA, secondary to recent insulin omission. You administer 12 units of rapid-acting insulin subcutaneously, encourage oral fluid intake and arrange for Michael’s transfer to your nearest tertiary centre via an ambulance.
Apart from urgent referral to the hospital, are there any additional management steps GPs could perform for cases of DKA?
The initial management of DKA involves fluid resuscitation and insulin administration.1 People with hyperglycaemia can develop polyuria and dehydration and, thus, adequate hydration is important. Regular consumption of oral fluids in small amounts (125 to 250 mL/h) should be encouraged. Ensuring the patient has access to water while waiting to present to the emergency department (ED) is important. If the patient is unable to tolerate oral fluids because of nausea or vomiting, intramuscular metoclopramide should be administered and GPs should consider calling an ambulance to provide intravenous fluids (0.9% sodium chloride at 500 to 1000 mL/h).
Given that DKA is usually managed with insulin infusion, is it better to wait until a patient’s situation can be closely monitored in the ED before administering insulin?
DKA arises because of insulin deficiency; therefore, patients with DKA benefit from the provision of insulin administered either subcutaneously or intravenously. Any dose of insulin administered while waiting to present to the ED will be beneficial, particularly if there is a history of insulin omission. In general, a subcutaneous rapid-acting insulin dose of 20% of the person’s total daily dose of insulin (TDD) can be safely given in a DKA emergency precipitated by insulin omission, and a dose of 10% of the TDD can be administered when all regular insulin has already been taken. For people with type 1 diabetes using insulin pen injections, the TDD is calculated by summing up all the usual injections (rapid-acting, long-acting and any mixed insulin); for people with type 1 diabetes on insulin pumps, the average TDD can be obtained from the pump in the pump history.
Blood glucose and ketone levels should be monitored every one to two hours. Outpatient sick day management plans from the Australian Diabetes Educator Association advises people with DKA to administer additional subcutaneous insulin every two hours to treat developing ketosis.2 DKA increases insulin resistance, and correction doses of subcutaneous insulin are higher compared with doses when ketones are not present.
Intravenous insulin infusions have long been the standard of care for DKA treatment.1 However, recent guidelines have suggested that subcutaneous insulin can be used to treat mild to moderate DKA effectively.3 If there is a delay in administering intravenous insulin, it is beneficial to administer subcutaneous insulin.
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are now being prescribed for type 2 diabetes, chronic kidney disease and heart failure. What special considerations are there when managing a person with type 1 diabetes prescribed SGLT-2 inhibitors?
SGLT-2 inhibitors (i.e. dapagliflozin, empagliflozin) are currently TGA approved and PBS listed in Australia for management of glycaemia in people with type 2 diabetes. DKA may occur in people with type 2 diabetes treated with SGLT-2 inhibitors in the context of acute metabolic stress, such as concurrent illness or prolonged fasting, but often at blood glucose levels of less than 15 mmol/L and hence known as euglycaemic DKA.
Multiple trials have demonstrated that SGLT-2 inhibitors, when used in people with type 1 diabetes, improve glycated haemoglobin levels, decrease glycaemic variability, reduce insulin requirements, lower weight and lower blood pressure, without increasing the risk of hypoglycaemia.4 However, there is an increased risk of DKA, with the US Food and Drug Administration estimating an eightfold higher risk of DKA in people with type 1 diabetes treated with SGLT-2 inhibitors.5 The TGA released a medication safety update in 2022, specifically highlighting that type 1 diabetes is not an approved indication for SGLT-2 inhibitors.6
DKA may occur at lower blood glucose levels (i.e. euglycaemic DKA with blood glucose levels <15 mmol/L) and, thus, ketone levels should be measured if there are signs or symptoms of ketosis (nausea, vomiting, abdominal pain, tachypnoea, drowsiness, fruity breath) even when the blood glucose level is not elevated.
Given the significant risks and off-label nature of their use, SGLT-2 inhibitors should only be prescribed for a selected cohort of people with type 1 diabetes under the supervision of a specialist endocrinologist.7 Education on the risk and signs and symptoms of DKA should be delivered, and appropriate sick day management information should be provided, including how and when to measure ketones, and how to treat elevated ketones.8
Furthermore, SGLT-2 inhibitors are approved for the treatment of chronic kidney disease and heart failure. If SGLT-2 inhibitors are being considered for people with type 1 diabetes for cardiorenal indications, an endocrinologist should be involved to assess whether they are suitable candidates and ensure they have received appropriate education to mitigate the risk of DKA.
What should be included in a sick day management plan?
Sick day management is a critical aspect of care for people with type 1 diabetes. Illness results in the release of stress hormones and changes in oral intake that can affect glycaemic levels and the risk of DKA.2 Sick day management should be discussed by the person’s endocrinologist during regular clinical reviews. Some endocrinologists (or diabetes services attached to tertiary public hospitals) may be available for people with type 1 diabetes to contact during illness to provide advice on management, which can prevent morbidity and the need for ED presentation or hospitalisation. Written instructions for sick day management may also be provided by either the endocrinologist or credentialed diabetes educator, providing clear guidance on personalised actions to take and assisting with self-management.2
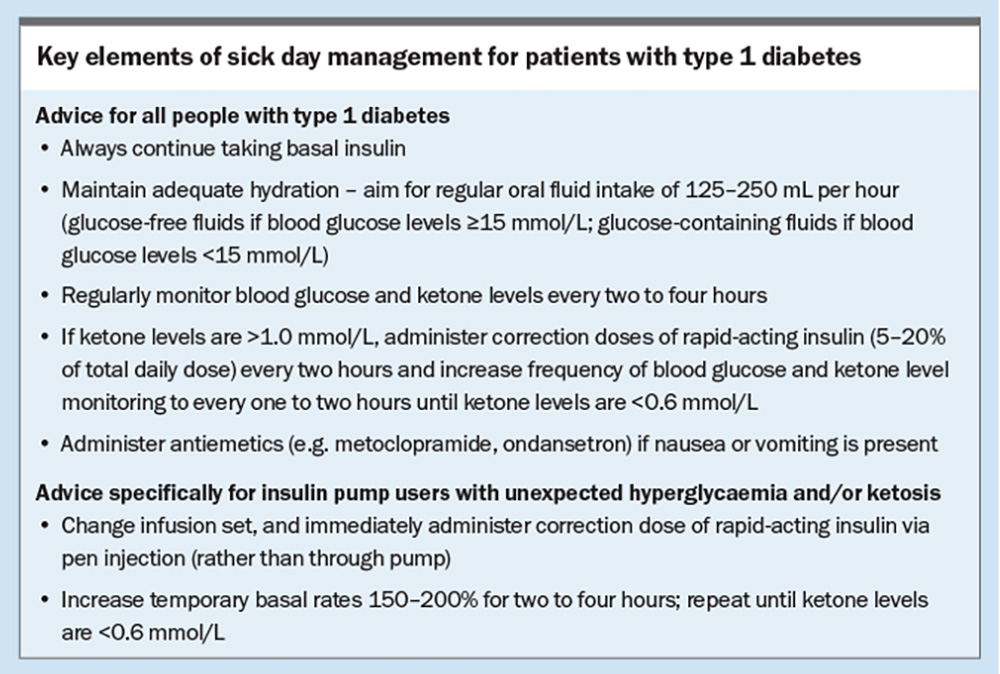
Key elements of sick day management include maintaining adequate hydration (glucose-free fluids if blood glucose levels are 15 mmol/L or higher; glucose-containing fluids if blood glucose levels are less than 15 mmol/L), regularly monitoring blood glucose and ketone levels every two to four hours, administering additional insulin for elevated ketones (>1.0 mmol/L, with or without hyperglycaemia) and taking antiemetic medications (e.g. oral ondansetron or intramuscular metoclopramide), which is often supported by their GP (Box). For people with type 1 diabetes in whom insulin pump failure or line occlusion may be a cause of unexpected hyperglycaemia and/or ketosis, education should include delivering a correction dose of rapid-acting insulin via pen injection to ensure insulin is delivered immediately, changing the reservoir and infusion set (tubing, cannula), and increasing the temporary basal rate to 150 to 200% for two to four hours.9
Which pumps are currently available in Australia, and what funding is available for people with type 1 diabetes to access these?
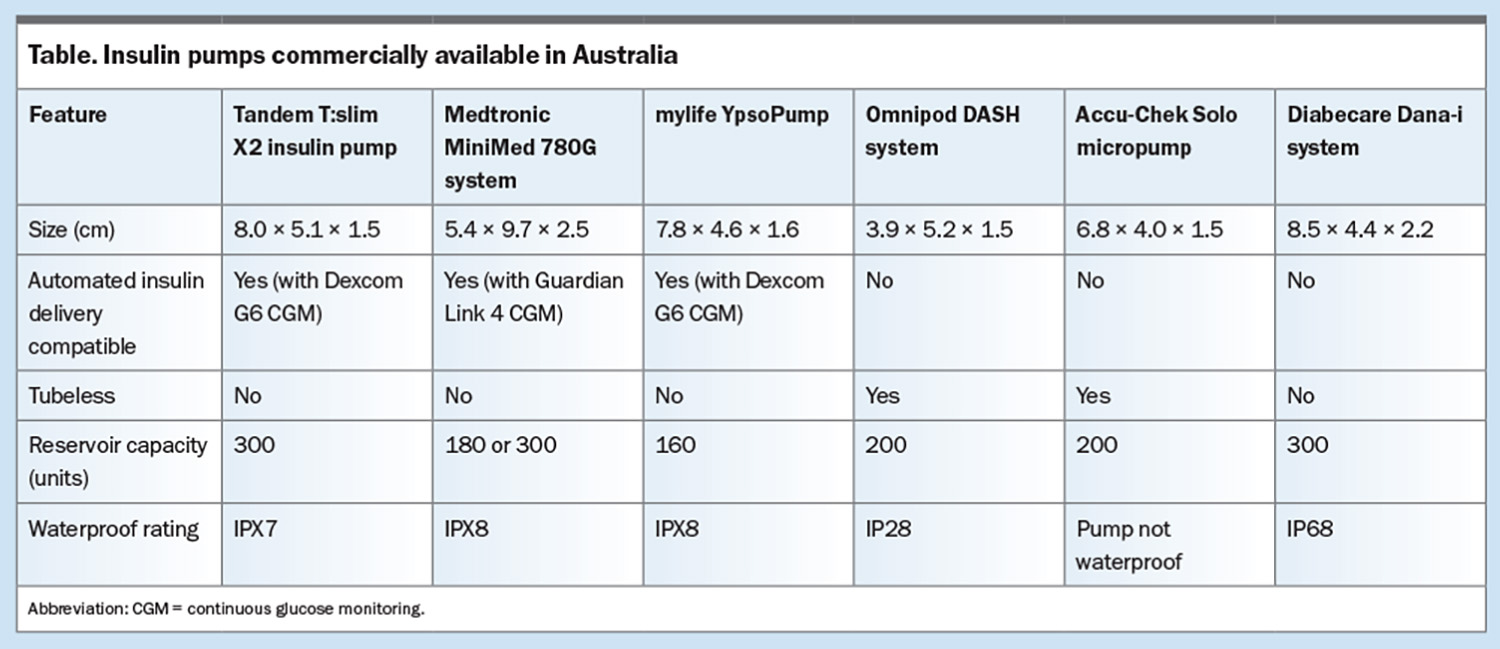
There are six insulin pumps available in Australia via private health insurance (Table). Older models of these pumps continue to be used by people with type 1 diabetes (e.g. Medtronic 640G/670G, DANA R, DANA RS, Roche Accu-Chek Combo), but these are being phased out and are not available for commencement. Additional insulin pump options exist overseas but these are not currently available in Australia.
Insulin pumps are expensive, and most people with type 1 diabetes using insulin pumps acquire them via private health insurance (with the level of coverage required for insulin pumps varying by health fund), with the ability to obtain a new insulin pump after four to five years depending on the health fund (although all warranties on pumps are for four years). People with type 1 diabetes aged younger than 21 years without private health insurance and a combined family income of $117,348 or less can apply to the Federal Government Insulin Pump Program, administered by the Juvenile Diabetes Research Foundation, which allows about 220 children and young people to access a fully subsidised insulin pump each year (currently the mylife YpsoPump).10
Do insulin pumps increase the risk of DKA?
There is mixed evidence regarding the relationship between the risk of DKA and use of insulin pump therapy.11-13 People with type 1 diabetes using insulin pumps do not use long-acting insulin, as the insulin pump only delivers rapid-acting insulin. Thus, any malfunction associated with the pump or infusion set (i.e. tubing, cannula) may result in absolute insulin deficiency and the progression to DKA within a few hours. Pump and infusion set-related issues are the most common precipitating factor for DKA in pump users, with a recent study estimating insulin pump users experience on average four faulty infusion set changes annually.14,15 DKA that arises because of an absence of insulin without intercurrent illness rapidly resolves on restoration of insulin delivery.
Nonetheless, improvements in insulin pump and infusion set technology, widespread uptake of continuous glucose monitoring (CGM) and enhanced patient education have changed the landscape. A recent large population-based, propensity-matched cohort study in Europe suggested decreased rates of DKA in people with type 1 diabetes treated with insulin pumps.11
Providing education to patients regarding the risk of pump failure and troubleshooting pump issues is critical. Practical tips to reduce the risk of pump failure-associated DKA include changing the infusion set if there is persistent unexplained hyperglycaemia, delivering rapid-acting insulin via pen injection to correct unexplained hyperglycaemia and avoiding infusion set changes prior to bedtime.
On resolution of DKA, what steps can be taken to reduce the future risk of DKA?
- Ensure the person with type 1 diabetes has a written sick day management plan and access to ketone strips and a ketone meter.
- Encourage regular insulin administration, particularly emphasising the importance of not omitting long-acting insulin when using pen injections under any circumstance
- Recommend CGM, which provides real-time glycaemic data, and assists people with type 1 diabetes to identify prolonged hyperglycaemia earlier, thereby preventing progression to DKA.
Studies have shown that CGM use reduces the risk of DKA in people with type 1 diabetes by 49 to 56%, reduces severe hypoglycaemia, improves glycaemic control and improves quality of life.16-18 The expansion of the Australian federal government subsidy for accessing CGM in July 2022 has reduced the cost of CGM to a maximum of $390 per annum for people with type 1 diabetes, with some groups eligible for full subsidy. Registration with the National Diabetes Services Scheme to access subsidised CGM can be completed by an endocrinologist, physician, paediatrician or credentialled diabetes educator.
Conclusion
DKA is a life-threatening emergency; prompt treatment with rapid-acting insulin and fluid hydration can prevent significant morbidity and mortality. All people with type 1 diabetes should have a sick day management plan to prevent the development of DKA. Diabetes technology, such as insulin pumps and CGM, are becoming increasingly used by people with type 1 diabetes, but these patients require specific education to both use these technologies and troubleshoot potential issues. ET
COMPETING INTERESTS: Dr Sriravindrarajah: None. Professor Holmes-Walker has received a grant from the Australian Diabetes Society in 2019, consulting fees from Ypsomed Australia and payment for HP education from Sanofi-Aventis; held a leadership role in the Australian Diabetes Society, 2014–2020; was Chair of the RACP Endocrinology Advanced Training Committee, 2018–2022; and is Chair of the Endocrinology Curriculum Review Committee, 2020–2024.
References
1. Umpierrez GE, Davis GM, ElSayed NA, et al. Hyperglycaemic crises in adults with diabetes: a consensus report. Diabetologia 2024 Jun 22; e-pub (https://doi.org/10.1007/s00125-024-06183-8).
2. Australian Diabetes Educators Association (ADEA). Managing sick days for adults with type 1 diabetes on insulin injections. Canberra: ADEA; 2020. Available online at: https://www.adea.com.au/wp-content/uploads/2020/09/Consumer_02_03.pdf (accessed July 2024).
3. American Diabetes Association Professional Practice Committee. 16. Diabetes Care in the Hospital: Standards of Care in Diabetes-2024. Diabetes Care 2024; 47: S295-S306.
4. Boeder S, Edelman SV. Sodium-glucose co-transporter inhibitors as adjunctive treatment to insulin in type 1 diabetes: a review of randomized controlled trials. Diabetes Obes Metab 2019; 210: 62-77.
5. Danne T, Garg S, Peters AL, et al. International consensus on risk management of diabetic ketoacidosis in patients with type 1 diabetes treated with sodium-glucose cotransporter (SGLT) inhibitors. Diabetes Care 2019; 42: 1147-1154.
6. Therapeutic Goods Administration (TGA). SGLT2 inhibitors approved for T2DM only. Canberra: TGA; 2022. Available online at: https://www.tga.gov.au/resources/publication/publications/sglt2-inhibitors-approved-t2dm-only (accessed July 2024).
7. Evans M, Hicks D, Patel D, Patel V, McEwan P, Dashora U. Optimising the benefits of SGLT2 inhibitors for type 1 diabetes. Diabetes Ther 2020; 11: 37-52.
8. Goldenberg RM, Gilbert JD, Hramiak IM, Woo VC, Zinman B. Sodium-glucose co-transporter inhibitors, their role in type 1 diabetes treatment and a risk mitigation strategy for preventing diabetic ketoacidosis: the STOP DKA protocol. Diabetes Obes Metab 2019; 21: 2192-2202.
9. University of Washington Medical Centre (UW Medicine). Insulin pumps and diabetic ketoacidosis (DKA). Washington, DC: UW Medicine; 2013. Available from: https://healthonline.washington.edu/sites/default/files/record_pdfs/Insulin-Pumps-Diabetic-Ketoacidosis-(DKA).pdf (accessed July 2024).
10. Juvenile Diabetes Research Foundation (JDRF). Insulin pump program 2024. Sydney: JDRF; 2024. Available online at: https://jdrf.org.au/living-with-t1d/insulin-pump-program/ (accessed July 2024).
11. Karges B, Schwandt A, Heidtmann B, et al. Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis, and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA 2017; 318: 1358-1366.
12. Hoshina S, Andersen GS, Jørgensen ME, Ridderstråle M, Vistisen D, Andersen HU. Treatment modality–dependent risk of diabetic ketoacidosis in patients with type 1 diabetes: Danish Adult Diabetes Database study. Diabetes Technol Ther 2018; 20: 229-234.
13. Pala L, Dicembrini I, Mannucci E. Continuous subcutaneous insulin infusion vs modern multiple injection regimens in type 1 diabetes: an updated meta-analysis of randomized clinical trials. Acta Diabetologica 2019; 56: 973-980.
14. Flores M, Amir M, Ahmed R, et al. Causes of diabetic ketoacidosis among adults with type 1 diabetes mellitus: insulin pump users and non-users. BMJ Open Diabetes Res Care 2020; 8: e001329.
15. Kanapka LG, Lum JW, Beck RW. Insulin pump infusion set failures associated with prolonged hyperglycemia: frequency and relationship to age and type of infusion set during 22,741 infusion set wears. Diabetes Technol Ther 2022; 24: 396-402.
16. Karges B, Tittel SR, Bey A, et al. Continuous glucose monitoring versus blood glucose monitoring for risk of severe hypoglycaemia and diabetic ketoacidosis in children, adolescents, and young adults with type 1 diabetes: a population-based study. Lancet Diabetes Endocrinol 2023; 11: 314-323.
17. Pickup JC, Freeman SC, Sutton AJ. Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. BMJ 2011; 343: d3805.
18. Roussel R, Riveline J-P, Vicaut E, et al. Important drop in rate of acute diabetes complications in people with type 1 or type 2 diabetes after initiation of flash glucose monitoring in France: the RELIEF study. Diabetes Care 2021; 44: 1368-1376.