Post-transplant diabetes mellitus: an individualised approach

Diabetes is common after solid organ transplantation. Organ transplant recipients are managed by specialist teams. However, as the number of transplantations increases and survival rates improve, the care of these patients will be increasingly shared with GPs and other physicians.
- Diabetes is common after solid organ transplantation.
- Insulin is the mainstay of treatment in the early post-transplant period, but thereafter management of post-transplant diabetes mellitus (PTDM) needs to be individualised.
- Patients with PTDM need standard monitoring for diabetes complications.
- In patients with PTDM, if the glucocorticoid dose is changed, glucose levels should be closely monitored and treatment titrated.
- As the number of transplantations increases and survival rates improve, the care of transplant recipients will be increasingly shared with GPs and other physicians.
Case scenario
Deborah, a 58-year-old woman living in rural Australia, attends your clinic. Her primary medical issue is dilated cardiomyopathy, which progressed over the past five years despite medical therapy to cause severe functional limitation. She underwent heart transplantation six months ago.
Despite normoglycaemia being demonstrated during the work-up for the transplantation, Deborah has developed post-transplant diabetes mellitus (PTDM). She required an insulin infusion in the intensive care unit immediately after the transplantation while receiving high-dose intravenous glucocorticoids. Her immunosuppressant regimen now includes tacrolimus, mycophenolate, everolimus and prednisolone 10 mg in the morning. She has also started taking isophane human insulin 20 units in the morning for diabetes.
Pathology results show her creatinine level is 105 micromol/L with an estimated glomerular filtration rate (eGFR) of 45 mL/min/1.73 m2. Her glycated haemoglobin (HbA1c) level is 7.1% (or 54 mmol/mol) and haemoglobin level is 114 g/L. Her urine albumin-to-creatinine ratio has not been measured recently.
How common is organ transplantation?
Solid organ transplantation (such as, kidney, liver, heart and lung) is a lifesaving procedure for end-stage organ disease. In Australia, there were 1396 solid organ transplants in 2023, including 829 kidney transplants, 287 liver transplants, 164 lung transplants and 129 heart transplants.1 Graft survival rates continue to improve, with Australian five-year survival at 74 to 87%.2 Subsequently, management of long-term complications is increasingly important.
What is PTDM and why does it occur?
PTDM is diabetes diagnosed after solid organ transplantation. It was previously termed ‘new-onset diabetes after transplant’ or NODAT.3 It occurs after acute stress and in the context of immunosuppressive medications.
Glucocorticoids, calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors prevent and treat rejection of the transplanted organ; however, these same medications are associated with the development of PTDM.4 Hyperglycaemia related to prednisolone therapy is dose dependent, with evidence of improvements in insulin sensitivity with steroid dose reductions down to 5 mg.5 However, once prednisolone dose is weaned to 5 mg daily, there may be no glycaemic benefit in further reduction. Additionally, a Cochrane review found steroid avoidance in renal transplant recipients increased the risk of acute transplant rejection without significant improvements in rates of diabetes.6
Calcineurin inhibitors, such as tacrolimus and cyclosporin, are associated with PTDM and beta-cell impairment, with tacrolimus exhibiting a stronger diabetogenic effect compared with cyclosporin.7 The use of mTOR inhibitors, such as sirolimus and everolimus, are also associated with PTDM, with sirolimus associated with an increased risk in delayed (five to 10 year) PTDM.7 Similar to the steroid effect, there is a dose-dependent effect of both calcineurin inhibitors and mTOR inhibitors on hyperglycaemia and diabetes.8
There are conflicting data on the role of switching immunosuppressant medications and PTDM risk; the choice of immunosuppressant should be individualised to the patient and graft survival prioritised over PTDM risk, with the lowest effective dose used to minimise side effects.9-11
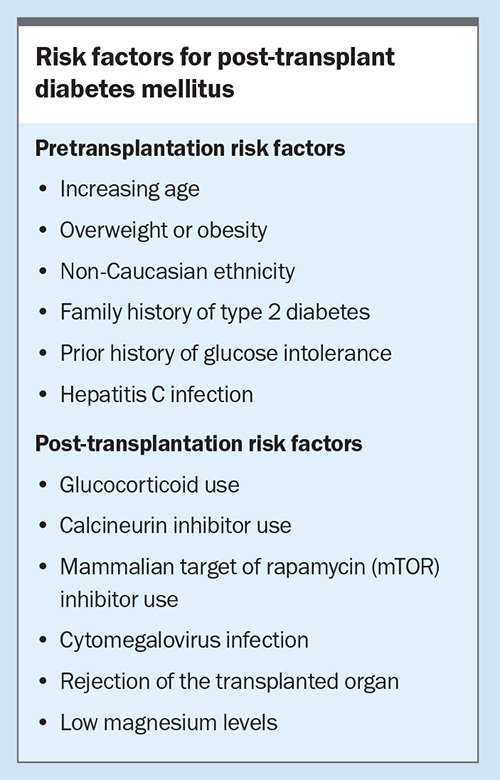
What are the predictors for PTDM?
Similarities exist between the pathogenesis of type 2 diabetes mellitus (T2DM) and PTDM. As with T2DM, insulin resistance and insulin deficiency often coexist in PTDM, as well as impaired suppression of hepatic glucose production.12-14 Obesity, older age and many other risk factors are shared between T2DM and PTDM, although additional transplant-specific risk factors, such as viral infections and hypomagnesaemia, exist for PTDM.15,16 Risk factors for PTDM are shown in the Box.
How soon does PTDM develop after a transplant and how is it diagnosed?
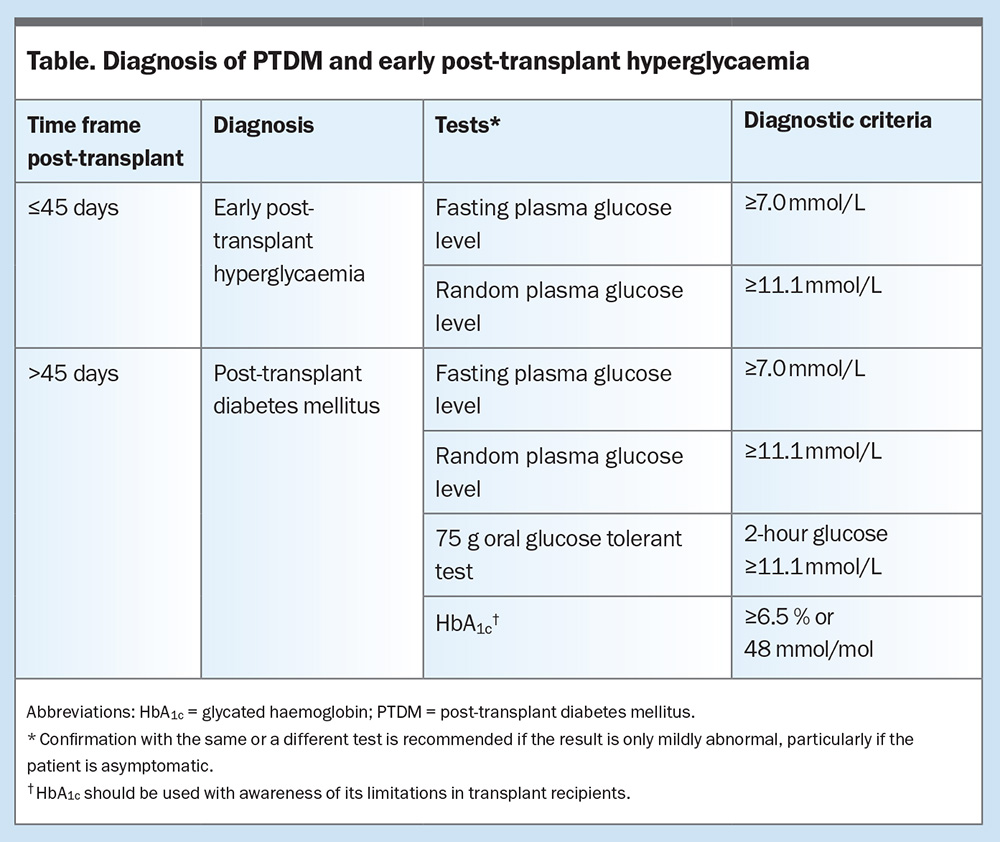
An international consensus guideline on PTDM was established at a meeting in Vienna, Austria, in 2013 to standardise the diagnosis of PTDM.3 To avoid a misdiagnosis of transient early post-transplant hyperglycaemia, a diagnosis of PTDM should be delayed until 45 days or six weeks after transplantation.3,9 Recently, there has also been a focus on early post-transplant hyperglycaemia, which occurs in the first 45 days post-transplant, as it is a strong predictor of PTDM.17,18 A summary of the diagnostic time frame for PTDM is shown in the Table.
The oral glucose tolerance test is the gold-standard tool for the diagnosis of PTDM;3 however, it may be impractical and unnecessary if hyperglycaemia is already established by another diagnostic criteria. As PTDM typically causes increased postprandial hyperglycaemia, a fasting glucose measurement may be normal.19,20 HbA1c measurement is a convenient test for screening for diabetes, but it has limitations in transplant recipients and may be spuriously normal due to anaemia, transfusion and other causes of reduced red blood cell survival.21-23
Most cases of PTDM are diagnosed in the first three months after transplantation; however, development of PTDM in subsequent years post-transplant has been reported.24 Hence, transplant recipients should be screened annually for PTDM.
What impact does PTDM have on transplant outcomes?
Early recognition and initiation of treatment of PTDM is important given that diabetes increases the risk of infection, graft failure and mortality after transplantation.24 Diabetes after heart transplantation is associated with coronary allograft vasculopathy and kidney disease progression.4
How does management differ between PTDM and other types of diabetes?
The choice of therapeutic agent in managing PTDM is often extrapolated from T2DM guidelines. Treatment is tailored to the individual taking into consideration the use of concomitant medications (particularly glucocorticoids), pattern of hyperglycaemia, likelihood of insulin secretion and sensitivity and avoidance of side effects.
In the early post-transplant period, insulin is the mainstay of treatment, because of its immediate action and safety profile.4 There is some evidence that in patients with hyperglycaemia in the postoperative phase, using basal insulin rather than bolus insulin may reduce the risk of developing PTDM, due to less glucose toxicity, beta-cell rest or both.25,26
Lifestyle optimisation remains an important factor in the long-term management of patients with PTDM. A balanced diet and adequate physical activity have been shown to improve glycaemic control in transplant recipients and should be encouraged at every healthcare encounter.27
Metformin is first-line therapy for T2DM in Australia and can be used in transplant recipients with preserved renal function. There is some evidence of cardiovascular benefits and reduced malignancy rates with metformin use in heart transplant recipients.4
Although there is established evidence of the cardiovascular and renal benefits of sodium-glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists in the management of T2DM, evidence in transplant recipients is limited to small and often retrospective studies.28-31 Renal impairment and cardiovascular disease are important comorbidities for transplant recipients; hence, these agents may have important benefits for this cohort and require further evaluation. Retrospective and small prospective studies have implied safety of these agents in transplant recipients and there are no known immunosuppression drug interactions.4,28,31,32 Potential side effects to be particularly cautious of are nausea and vomiting with GLP-1 receptor agonists and genitourinary infections and diabetic ketoacidosis risk with SGLT-2 inhibitors.33
Gliclazide, a sulfonylurea, has traditionally been used as an alternative to insulin to treat glucocorticoid-induced hyperglycaemia.34 There is limited evidence on its safety and efficacy in PTDM. There is a possible interaction with CYP2C9 inhibitors (such as fluconazole, trimethoprim and metronidazole), which may be used to manage infections; this may result in reduced metabolism of gliclazide and increased risk of hypoglycaemia.32
Dipeptidyl peptidase-4 (DPP-4) inhibitors are another class of diabetes medications with data supporting safety and efficacy in improved glycaemic control.35 DPP-4 inhibitors do not have cardiorenal benefits; however, there are emerging data about a possible association with allograft protection in lung transplantation.36 DPP-4 inhibitors can be used in the presence of renal impairment, for example linagliptin does not require renal dose adjustment.
If glucocorticoid doses change, or if a patient requires a pulse of glucocorticoids for rejection, glucose levels should be closely monitored and treatment will likely need to be escalated (usually with insulin). This also applies to a reduction in glucocorticoid dose, as there is risk of hypoglycaemia necessitating a reduction in pharmacological treatment, particularly if insulin or a sulfonylurea is being used.
What aspects of management can be facilitated in general practice?
Similar to the management of T2DM, the aims of PTDM management are optimising glycaemic results and monitoring and managing complications of hyperglycaemia. If the patient is prescribed insulin, capillary glucose levels should be routinely reviewed to ensure minimisation of hypoglycaemia (glucose levels <4 mmol/L) and hyperglycaemia (glucose levels >10 mmol/L). Currently, people living with PTDM do not qualify for subsidisation of continuous glucose monitors in Australia. In patients who are not taking insulin regular capillary glucose monitoring may not be required. HbA1c testing, acknowledging the previously mentioned limitations, may be used with caution to monitor glycaemia.
Screening for complications of diabetes includes annual urine albumin-to-creatinine ratio measurement; examination of the feet, assessing for peripheral pulses and sensation; and retinopathy screening. Additionally, annual review of cardiovascular risk factors, including measurement of blood pressure and cholesterol levels, should occur. Co-ordinating and ensuring multidisciplinary care is key and General Practitioner Management Plans are a great resource (see Services Australia’s online information on preparing a General Practitioner Management Plan at https://www.servicesaustralia.gov.au/prepare-gpmp-tcas-or-mhcc?context=20).
Is specialist referral required and when is this indicated?
Transplant recipients require closely integrated care between GPs in the community and highly specialised transplant units. Inclusion of an endocrinologist in this team serves to address metabolic and bone health in the high-risk patient, with proposed advantages including greater efficiency of care, improved quality of life, lower hospital admission rates and improved survival. Due to the complexity of solid organ transplants, it is recommended that all transplant recipients with diabetes be referred to an endocrinologist.
Case update
Over the following six months, Deborah’s prednisolone dose was reduced slowly to 5 mg. She was able to be weaned off insulin and was commenced on metformin 500 mg daily and empagliflozin 10 mg daily, with her glucose levels ranging from 5 to 10 mmol/L. Annual complication screening did not reveal any evidence of microalbuminuria, neuropathy or retinopathy.
Conclusion
Diabetes is common after solid organ transplantation and it increases the risk of infection, graft failure and mortality. Hence, early recognition is important. Management of patients with PTDM is individualised and includes lifestyle modification, use of antiglycaemic agents and insulin, risk-reduction strategies and screening for complications. Transplant recipients need closely integrated care between GPs and highly specialised transplant units. ET
COMPETING INTERESTS: Dr Raven has received a PhD scholarship from the Heart Foundation. Professor Greenfield has received study drug and placebo from Novo Nordisk for a study of semaglutide in type 1 diabetes and speaker fees from Novartis, Novo Nordisk, Amgen, Allergan, Boehringer Ingelheim, Lilly, Abbott and the Limbic.
References
1. Opdam H, Davies C, Marshall K, Irish G. 28th Report, Section 1: Snapshot of Deceased Organ Donation Activity in Australia and New Zealand. Adelaide: Australia and New Zealand Organ Donation Registry; 2024. Available online at: https://www.anzdata.org.au/wp-content/uploads/2024/05/s01_summary_2023_ar_2024_v1.0_F.pdf (accessed October 2024).
2. Australia and New Zealand Organ Donation Registry. 2019 Annual Report, Section 12: Deceased organ transplant outcome data. Adelaide: Australia and New Zealand Dialysis and Transplant Registry; 2019. Available online at: https://www.anzdata.org.au/report/anzod-annual-report-2019 (accessed October 2024).
3. Sharif A, Hecking M, de Vries APJ, et al. Proceedings from an international consensus meeting on posttransplantation diabetes mellitus: recommendations and future directions. Am J Transplant 2014; 14: 1992-2000.
4. Raven LM, Muir CA, Macdonald PS, Hayward CS, Jabbour A, Greenfield JR. Diabetes medication following heart transplantation: a focus on novel cardioprotective therapies—a joint review from endocrinologists and cardiologists. Acta Diabetol 2023; 60: 471-480.
5. Midtvedt K. Insulin resistance after renal transplantation: the effect of steroid dose reduction and withdrawal. J Am Soc Nephrol 2004; 15: 3233-3239.
6. Haller MC, Royuela A, Nagler EV, Pascual J, Webster AC. Steroid avoidance or withdrawal for kidney transplant recipients. Cochrane Database Syst Rev 2016; 2016: CD005632.
7. Kotha S, Lawendy B, Asim S, et al. Impact of immunosuppression on incidence of post-transplant diabetes mellitus in solid organ transplant recipients: systematic review and meta-analysis. World J Transplant 2021; 11: 432-442.
8. Newman JD, Schlendorf KH, Cox ZL, et al. Post-transplant diabetes mellitus following heart transplantation. J Heart Lung Transplant 2022; 41: 1537-1546.
9. Chowdhury TA, Wahba M, Mallik R, et al. Association of British Clinical Diabetologists and Renal Association guidelines on the detection and management of diabetes post solid organ transplantation. Diabetic Med 2021; 38: e14523.
10. Cehic MG, Nundall N, Greenfield JR, Macdonald PS. Management strategies for posttransplant diabetes mellitus after heart transplantation: a review. J Transplant 2018; 2018: 1025893.
11. Raven LM, Muir CA, Pouliopoulos J, et al. Metabolic sequelae of everolimus treatment after cardiac transplant: a hypothesis-generating study. Heart Lung Circ 2023; 32: 1076-1079.
12. Ekstrand AV, Eriksson JG, Grönhagen-Riska C, Ahonen PJ, Groop LC. Insulin resistance and insulin deficiency in the pathogenesis of posttransplantation diabetes in man. Transplantation 1992; 53: 563-569.
13. Hjelmesaeth J, Hagen M, Hartmann A, Midtvedt K, Egeland T, Jenssen T. The impact of impaired insulin release and insulin resistance on glucose intolerance after renal transplantation. Clin Transplant 2002; 16: 389-396.
14. Jørgensen MB, Hornum M, van Hall G, et al. The impact of kidney transplantation on insulin sensitivity. Transpl Int 2017; 30: 295-304.
15. Zhang M, Han Y, Yuan Y, et al. Risk factors for new-onset diabetes mellitus after heart transplantation in Chinese patients: a single center experience. Ann Nutr Metab 2019; 74: 331-338.
16. Zielińska K, Kukulski L, Wróbel M, Przybyłowski P, Zakliczyński M, Strojek K. Prevalence and risk factors of new-onset diabetes after transplantation (NODAT). Ann Transplant 2020; 25: e926556.
17. Kuang W, Raven LM, Muir CA. Early post-transplant hyperglycemia and post-transplant diabetes mellitus following heart transplantation. Expert Rev Endocrinol Metab 2024; 19: 129-140.
18. Iqbal A, Zhou K, Kashyap SR, Lansang MC. Approach to the patient: early post-renal transplant hyperglycemia. J Clin Endocrinol Metab 2021 Sep 24; dgab697.
19. Sharif A, Moore RH, Baboolal K. The use of oral glucose tolerance tests to risk stratify for new-onset diabetes after transplantation: An underdiagnosed phenomenon. Transplantation. 2006 Dec 27;82(12):1667–1672.
20. Valderhaug TG, Jenssen T, Hartmann A, et al. Fasting plasma glucose and glycosylated hemoglobin in the screening for diabetes mellitus after renal transplantation. Transplantation 2009; 88: 429-434.
21. Eide IA, Halden TAS, Hartmann A, et al. Limitations of hemoglobin A1c for the diagnosis of posttransplant diabetes mellitus. Transplantation 2015; 99: 629-635.
22. Pimentel AL, Cavagnolli G, Camargo JL. Diagnostic accuracy of glycated hemoglobin for post-transplantation diabetes mellitus after kidney transplantation: systematic review and meta-analysis. Nephrol Dial Transplant 2017; 32: 565-572.
23. Yates CJ, Fourlanos S, Colman PG, Cohney SJ. Screening for new-onset diabetes after kidney transplantation: limitations of fasting glucose and advantages of afternoon glucose and glycated hemoglobin. Transplantation 2013; 96: 726-731.
24. Jenssen T, Hartmann A. Post-transplant diabetes mellitus in patients with solid organ transplants. Nat Rev Endocrinol 2019; 15: 172-188.
25. Hecking M, Haidinger M, Döller D, et al. Early basal insulin therapy decreases new-onset diabetes after renal transplantation. J Am Soc Nephrol 2012; 23: 739-749.
26. Bhat M, Usmani SE, Azhie A, Woo M. Metabolic consequences of solid organ transplantation. Endocrine Reviews 2021; 42: 171-197.
27. Sharif A, Moore R, Baboolal K. Influence of lifestyle modification in renal transplant recipients with postprandial hyperglycemia. Transplantation 2008; 85: 353-358.
28. Cehic MG, Muir CA, Greenfield JR, et al. Efficacy and safety of empagliflozin in the management of diabetes mellitus in heart transplant recipients. Transplant Direct 2019; 5: e450.
29. Halden TAS, Kvitne KE, Midtvedt K, et al. Efficacy and safety of empagliflozin in renal transplant recipients with posttransplant diabetes mellitus. Diabetes Care 2019; 42: 1067-1074.
30. Sammour Y, Nassif M, Magwire M, et al. Effects of GLP-1 receptor agonists and SGLT-2 inhibitors in heart transplant patients with type 2 diabetes: Initial report from a cardiometabolic center of excellence. J Heart Lung Transplantation 2021; 40: 426-429.
31. Singh P, Taufeeq M, Pesavento TE, Washburn K, Walsh D, Meng S. Comparison of the glucagon-like-peptide-1 receptor agonists dulaglutide and liraglutide for the management of diabetes in solid organ transplant: A retrospective study. Diabetes Obes Metab 2020; 22: 879-884.
32. Vanhove T, Remijsen Q, Kuypers D, Gillard P. Drug-drug interactions between immunosuppressants and antidiabetic drugs in the treatment of post-transplant diabetes mellitus. Transplant Rev (Orlando) 2017; 31: 69-77.
33. Raven LM, Cao JY, Macdonald PS, Jabbour A, Greenfield JR. Fournier’s gangrene in recent transplant recipient on empagliflozin. JHLT Open [Internet] 2024; 4C: 100060. Available online at: https://www.jhltopen.org/article/S2950-1334(24)00009-0/fulltext (accessed October 2024).
34. Roberts A, James J, Dhatariya K; Joint British Diabetes Societies (JBDS) for Inpatient Care. Management of hyperglycaemia and steroid (glucocorticoid) therapy: a guideline from the Joint British Diabetes Societies (JBDS) for Inpatient Care group. Diabetic Med 2018; 35: 1011-1017.
35. Sharif A, Chakkera H, de Vries APJ, et al. International consensus on post-transplantation diabetes mellitus. Nephrol Dial Transplant 2024; 39: 531-549.
36. Yamada Y, Sato T, Oda H, et al. Favorable effect of CD26/DPP-4 inhibitors on postoperative outcomes after lung transplantation: A propensity-weighted analysis. J Heart Lung Transplant 2024; 43: 66-76.