Managing atherosclerotic risk in type 1 diabetes

Type 1 diabetes is associated with accelerated atherosclerosis and increased cardiovascular disease (CVD) risk. Early recognition and aggressive treatment of traditional and emerging modifiable risks factors contribute to optimal management of atherosclerotic risk in people with diabetes. There is increasing recognition that CVD risk management in type 1 diabetes should be the same as for type 2 diabetes. Shared care involving a multidisciplinary team that includes specialists and allied healthcare professionals, and is co-ordinated by the patient’s GP, is the recommended management approach.
- People with type 1 diabetes have premature, accelerated atherosclerosis, with a high (greater than two- to fourfold) risk of cardiovascular disease (CVD) events and premature death relative to their peers without diabetes.
- CVD risk is often underestimated in type 1 diabetes and specific CVD risk calculators for people with type 1 diabetes are available.
- International guidelines for CVD risk management in diabetes no longer distinguish between type 1 and type 2 diabetes.
- Multiple risk factor targets and treatment strategies for people with type 1 diabetes are at least as aggressive as those for people with type 2 diabetes.
- Early recognition and initiation of risk factor control can improve life expectancy by up to 20 years.
Of the estimated 136,000 people in Australia with type 1 diabetes, about two-thirds are aged 40 years or older and about one-third are aged 60 years or older.1 These are the ages at which atherosclerosis-related clinical events typically manifest. In advantaged countries, atherosclerosis often begins in childhood and progresses subclinically over decades, with atherosclerotic plaque rupture and thrombosis precipitating clinical events. Although the heightened atherosclerosis risk in people with type 2 diabetes is well recognised, the risk for people with type 1 diabetes is often less well-recognised, including by many patients and clinicians. This article reviews the reasons for accelerated atherosclerosis in type 1 diabetes, suggests risk factor targets and treatments, and outlines the benefits of team care.
Why are people with type 1 diabetes at high risk of atherosclerosis?
Cardiovascular disease (CVD) is a major cause of morbidity, and the cause of death in 25% of people with type 1 diabetes.2-4 Atherosclerosis may manifest as coronary artery disease (CAD), cerebrovascular disease or peripheral vascular disease. The first manifestations of CAD include angina, heart failure or myocardial infarction, and are often fatal. Due to autonomic neuropathy, cardiac ischaemia in people with diabetes may be silent or atypical, the latter leading to non-diagnosis of CAD or an incorrect diagnosis such as gastroesophageal reflux.
Compared with those without diabetes, atherosclerosis in people with type 1 diabetes is often accelerated, starting at a younger age (e.g. in childhood), progressing more rapidly, extending more distally and being more diffuse and generalised. As such, surgical interventions, including bypass grafts and stents, are often more difficult and, sometimes, impossible to implement.2-4 The atherosclerotic plaque in people with diabetes is usually also lipid-rich and more inflamed and, therefore, more likely to rupture, triggering thrombosis and an acute vascular event.2,5,6 Women with type 1 diabetes, even those who are premenopausal, lose the cardioprotection that is evident in women without diabetes, and have a relative risk of CVD higher than that for men. Some subgroups, such as those with type 1 diabetes onset at younger than 10 years of age, are at particularly high risk for CVD (hazard ratio [HR], 11.4; range, 7.9 to 16.4), coronary heart disease (HR, 30.5; range, 20.0 to 46.67), acute myocardial infarction (HR, 31.0; range, 17.6 to 54.4) and stroke (HR, 6.4; range, 4.0 to 10.3).7
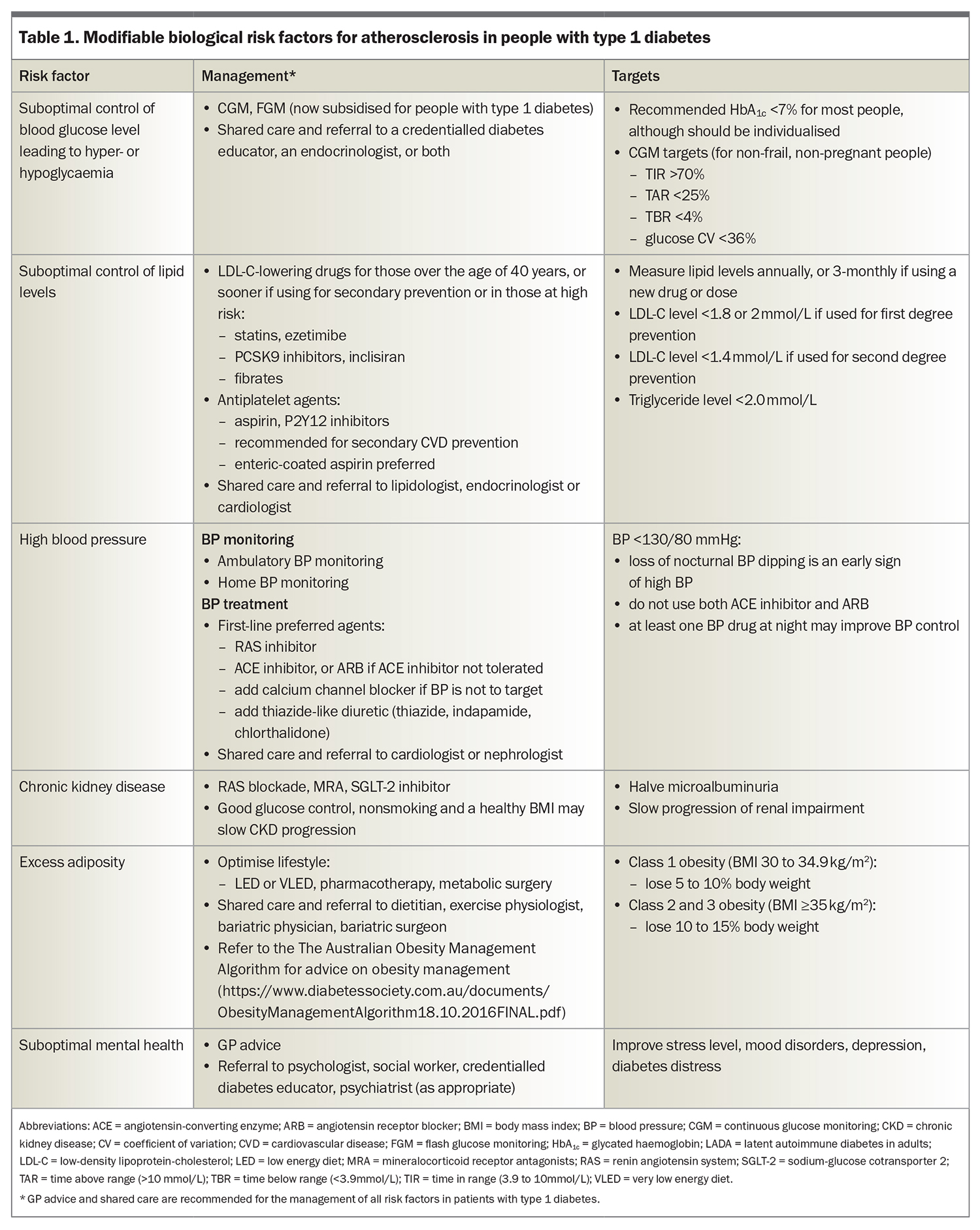
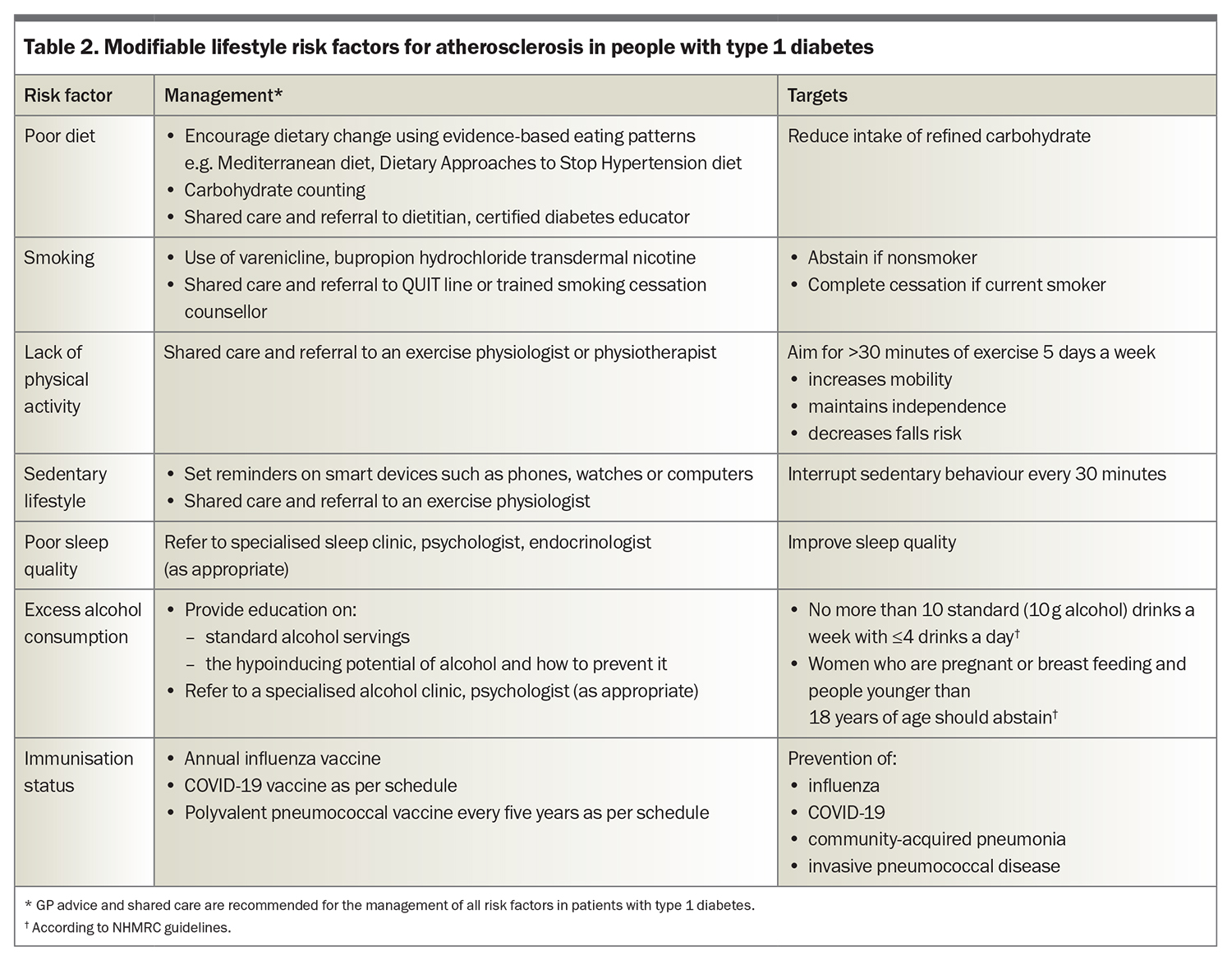
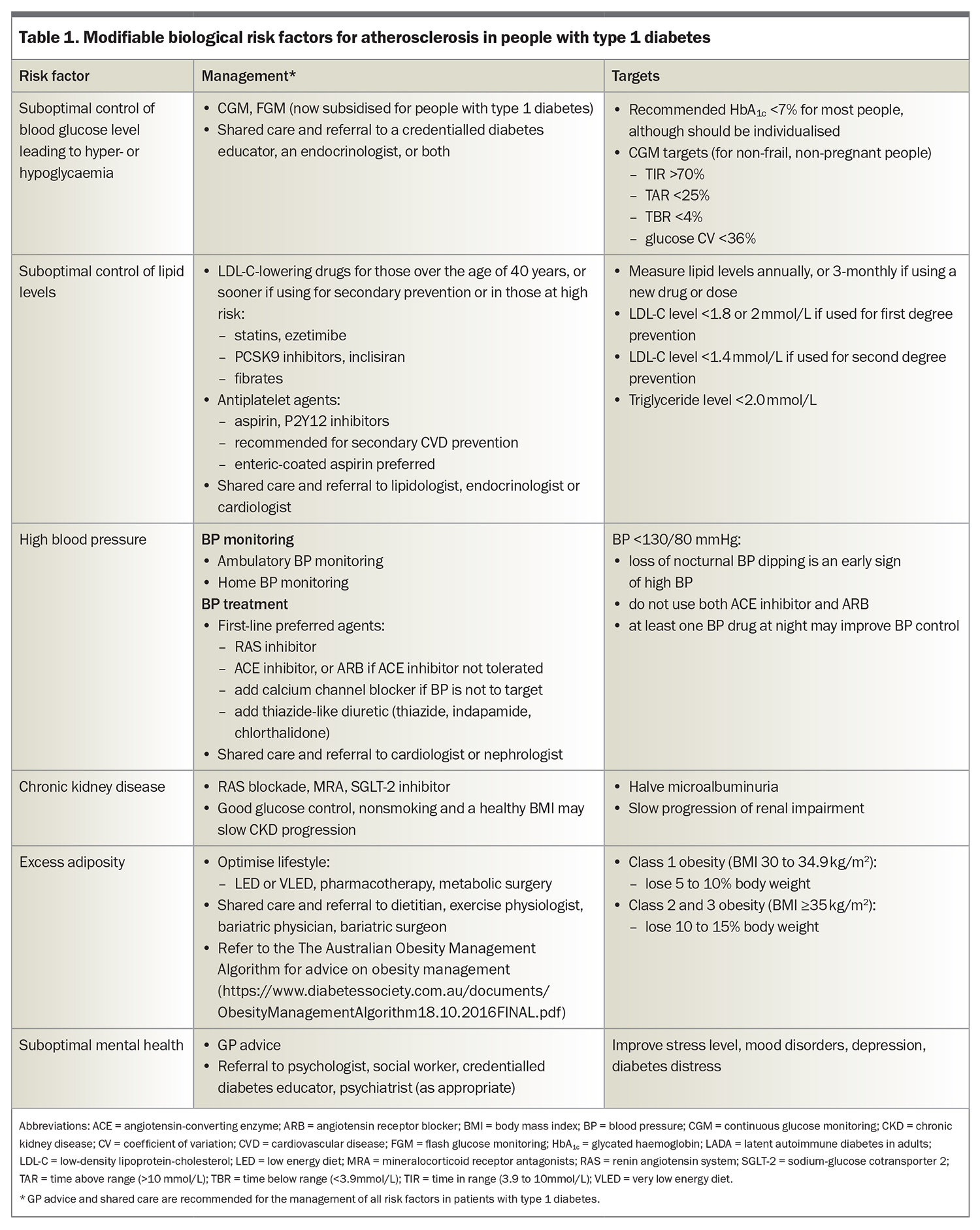
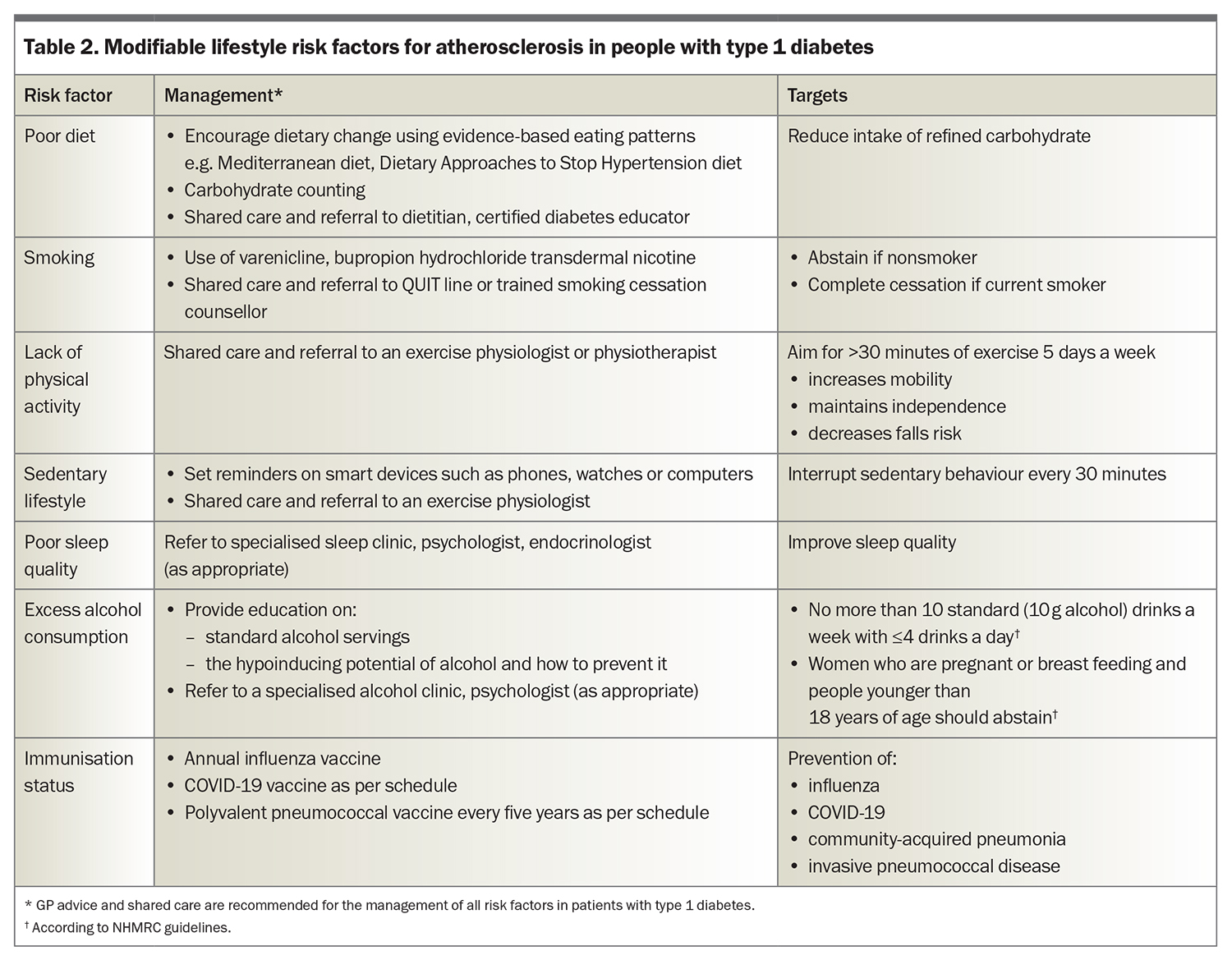
People with type 1 diabetes are also at high atherosclerotic risk if they have a family history of CVD in relatives with or without diabetes, or have microvascular complications of diabetes, coexisting obesity or insulin resistance (i.e. coexistent features of type 2 diabetes), which is also known as ‘double diabetes’.2,7-10 Adjunct metformin therapy may be helpful to retard atherosclerosis.9,10 In adults aged 20 to 50 years with type 1 diabetes, optimal risk factor control has been estimated to improve life expectancy by up to 20 years and the related risk factors, outlined in Table 1 and Table 2, may guide clinical discussions and patient education.7
Risk factors and mechanisms of atherosclerosis
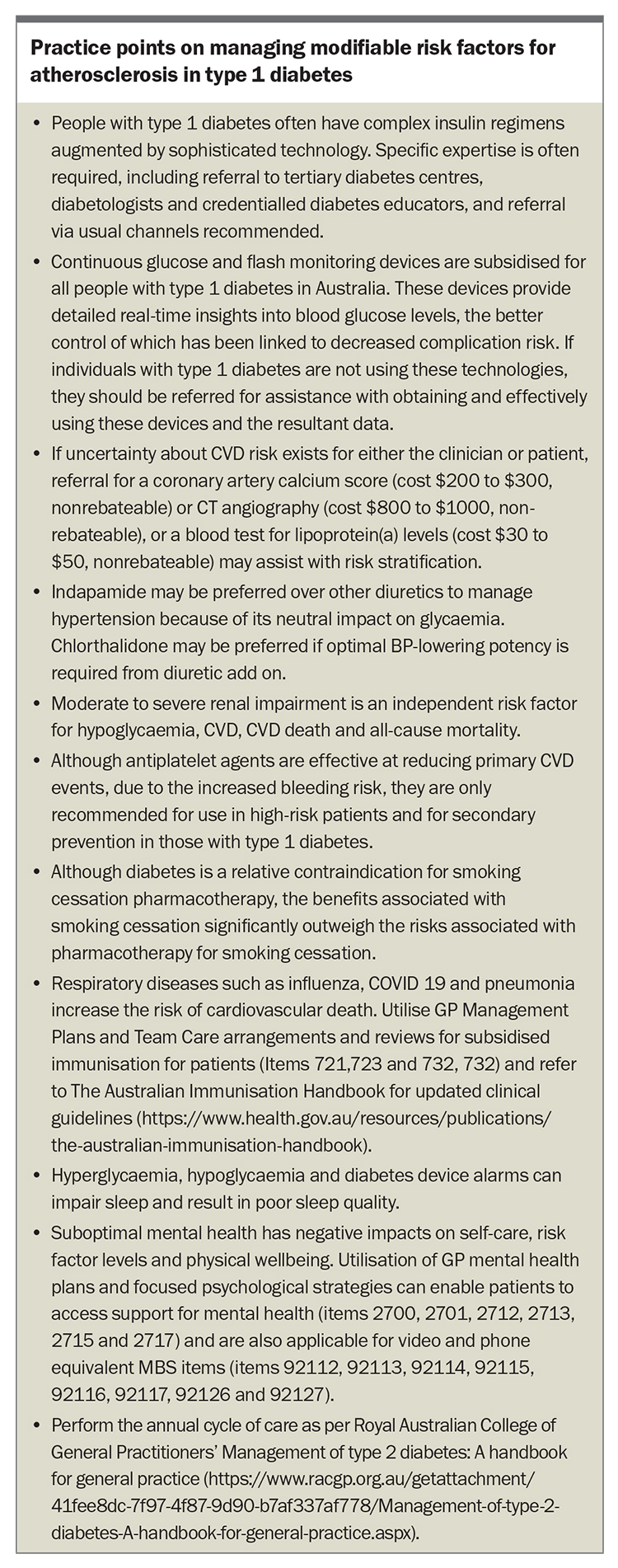
Traditional risk factors for atherosclerosis in people with type 1 diabetes include increasing age, long diabetes duration, hypertension, dyslipidaemia, smoking, being overweight or obese (with increasing prevalence) and hyperglycaemia (reflected by elevated glycated haemoglobin [HbA1c] levels). More recently, hypoglycaemia and glucose variability (greater fluctuations in glucose or HbA1c levels), have been identified as modifiable risk factors associated with an increased risk of vascular disease, with potential mechanisms including endothelial dysfunction, inflammation, thrombosis and oxidative stress.2,11-15 The pathophysiological processes, which involve novel vascular risk factors, can last for days, even after a nonsevere hypoglycaemic event. The Box summarises key practice points on managing modifiable risk factors for atherosclerosis in type 1 diabetes.
Type 1 diabetes is associated with vascular endothelial dysfunction related to reduced bioavailability of vasodilatory nitric oxide; increased inflammation and a prothrombotic status due to enhanced platelet adhesiveness and aggregability, increased clotting activity and impaired fibrinolysis; increased oxidative stress; and the formation of advanced glycation end products. The peripheral hyperinsulinaemia arising from subcutaneous insulin delivery is also thought to be proatherogenic, partly due to the induction of insulin resistance, which can be further aggravated by adiposity and a lack of exercise.2,8 Importantly, Swedish Diabetes Registry data showed that insulin delivery by a pump, rather than by multiple daily injections, was associated with a 40% reduction in CVD mortality, even for the same mean HbA1c level. This reduction may be related to a lower daily insulin dose, reduced number of hypoglycaemic episodes and less glucose variability associated with pump delivery.16
Although people with type 1 diabetes have relatively high HDL-cholesterol (HDL-C) levels and lower than average triglyceride levels (compared with those without diabetes) driven by peripheral hyperinsulinaemia, they are still at high CVD risk. This risk is related to qualitative changes in their lipoproteins, including from glycation, oxidation, the formation of advanced glycation end products and immune complexes, and a shift towards highly proatherogenic small dense LDL and dysfunctional HDL.2,17,18 Nevertheless, people with type 1 diabetes benefit from the use of antilipid drugs to the same level as those with type 2 diabetes and without diabetes.19 A meta-analysis by the Cholesterol Treatment Trialist Collaboration showed that people with type 1 diabetes on statin therapy had the same five-year reduction in CVD and mortality events as those with type 2 diabetes and the general population taking statins.19
Early renal dysfunction in type 1 diabetes is associated with increased CVD risk. This may relate to common risk factors for micro- and macrovascular damage, such as obesity, smoking, hypertension, hyperglycaemia (a stronger risk factor for microvascular events) and dyslipidaemia (a stronger risk factor for macrovascular events). Microalbuminuria alone is associated with proatherogenic changes in lipids and blood clotting.2,20
Atherosclerosis is an inflammatory condition and its development and progression, even in the general population, are enhanced by infection and inflammation, such as periodontal disease and SARS-CoV-2 infection. People with type 1 diabetes who have had COVID-19 have an increased CVD risk for up to a year after infection.21 This underpins the importance of good dental hygiene, regular dental check-ups and vaccinations. A potential role for colchicine, a potent anti-inflammatory drug, to reduce CVD risk in type 1 diabetes has been suggested but is not yet included in clinical guidelines.22
In both the general population and in those with type 1 diabetes, unmodifiable genetic risk factors may also contribute to atherosclerosis. Risk factors include a family history of CVD, dyslipidaemia or hypertension, and adverse genetic or polygenic risk scores on genetic profiling. The latter is currently used as a research tool but is becoming increasingly available for clinical use.
CVD risk scores for the general population and those with type 2 diabetes are not well-validated in people with type 1 diabetes, with emerging data suggesting CVD risk is underestimated.23,24 The Steno T1 Risk Engine (http://www.sdcc.dk/T1riskengine) is a free risk calculator for people with type 1 diabetes to predict the five- and 10-year risk of nonfatal and fatal CVD (CAD, stroke, peripheral vascular disease) and end-stage kidney disease.24 The risk engine has been validated using clinical data from about 5000 patients with type 1 diabetes from the Steno Diabetes Center Copenhagen, as well as data from the Danish National Patient Register and Cause of Death Register. The Steno risk engine scores also correlate with the presence of preclinical carotid atheroma.25 Noninvasive assessments of the arterial tree (e.g. carotid intima media thickness), cardiac function (e.g. echocardiography), coronary artery calcification (CAC) scores and CT-coronary angiography can also be useful to assess and monitor atherosclerosis status; however, CAC scores and CT-coronary angiograms are not PBS subsidised in Australia. An advantage of CT-coronary angiography is that it can potentially detect both stable and unstable plaque, although its power to discriminate between the two remains controversial.
Risk factor targets and treatments
Given the multiple risk factors for atherosclerosis and its slow development, patient with type 1 diabetes require education and support and regular monitoring, diagnostic tests, risk factor assessments and treatments. Epidemiological data from over 32,000 people with type 1 diabetes support the importance of identifying traditional risk factors and the benefits of aggressive management.26 A large observational study showed that the use of antilipid therapy in type 1 diabetes was associated with a 22 to 44% reduction in the risk of primary CVD events and cardiovascular death.27 Involving other healthcare professionals can benefit patient outcomes, and GPs routinely co-ordinate this shared care to manage atherosclerosis risk and CVD in people with type 1 diabetes. Often, repeated discussions are needed to help patients understand, achieve and maintain their treatment goals.
International guidelines for CVD risk management in diabetes no longer distinguish between type 1 and type 2 diabetes and, in general, risk factor targets and treatments for type 1 diabetes are similar to those for type 2 diabetes. The presence of multiple risk factors is often compounded by increasing age, type 1 diabetes duration and genetic risk factors, such that, even mild abnormalities of modifiable risk factors can promote atherosclerosis, and merit treatment. Modifiable risk factors, including dysglycaemia, lipids and blood pressure (BP), should be treated adequately and lifestyle factors optimised, including optimising weight and nutrition, promoting exercise and encouraging smoking cessation. Key management tools and strategies and recommended targets for modifiable biological and lifestyle risk factors for atherosclerosis in type 1 diabetes are outlined in Table 1 and Table 2, respectively.
The recent subsidy for continuous glucose monitoring (CGM) devices for people in Australia with type 1 diabetes may assist with reaching and maintaining glucose targets. As noted above, although insulin pump use (vs multiple daily injections) is associated with major reductions in CVD mortality,16 pump acquisition requires private health insurance, self-payment or philanthropy.
Pharmacotherapy is often needed to reach recommended lipid targets, with LDL-cholesterol (LDL-C)-lowering drugs (usually initially a statin) recommended for high-risk adults with type 1 diabetes and for those aged 40 years or older, independent of lipid levels. Because of the HDL dysfunction that occurs in type 1 diabetes,18 a normal or high HDL-C level or favourable LDL-C/HDL-C ratio should not be a reason to delay initiating LDL-C-lowering drugs. Such LDL-C-lowering drugs are not suitable for pregnant or breast-feeding women.
If statins are contraindicated, or not accepted or tolerated by patients, guidelines on statin intolerance may be helpful for clinicians in selecting alternative non-statin LDL-C-lowering drugs, including ezetimibe, PCSK9 inhibitors, inclisiran and the adenosine triphosphate-citrate lyase inhibitor bempedoic acid (not yet available in Australia).28 The Reduce Cardiovascular Events in High-Risk Patients With Hypertriglyceridemia and on Statin (REDUCE IT) trial showed high-dose eicosapentaenoic acid was effective for the secondary prevention of CVD events in people with high triglyceride levels; however, fewer than 1% of participants had type 1 diabetes and hypertriglyceridaemia is uncommon in type 1 diabetes.29
Patients with hypertension should be advised that more than one BP-lowering drug may be needed to reach recommended BP targets. In addition, BP is often better controlled across the day if at least one BP-lowering tablet is taken at bedtime.30 Clinicians should check the patient’s electrolyte levels and renal function after starting or up-titrating BP medications, in particular renin-angiotensin system (RAS) and mineralocorticoid receptor antagonist (MRA) medications, to ensure there is no hyperkalaemia. Resistant hypertension is not uncommon in people with diabetes and may merit further investigations or specialist referral.30
Benefits of shared care
Most GPs have few patients with type 1 diabetes, and they may be the only healthcare professional who some patients see. However, such patients should ideally be managed in a multidisciplinary setting, that includes close collaboration with the patient’s GP. Multidisciplinary care co-ordinated by the GP can facilitate patients achieving risk factor targets and mitigate primary and secondary atherosclerotic events. An endocrinologist, a diabetes nurse educator and a dietitian are crucial members of the multidisciplinary team. Other specialists, such as a cardiologist, nephrologist, neurologist or vascular surgeon or, for those with obesity, an obesity physician and bariatric surgery team may also be key team members.31,32 Allied healthcare professionals, including a dietitian, credentialled diabetes educator, psychologist, dentist and an exercise physiologist can also provide crucial input on patient management. A Care Plan can help minimise patient costs. A pharmacist can assist with complex treatment adherence, for example, through patient education, the provision of Webster packs and a free home medicines review, which can include checking devices for BP and blood glucose and ketone monitoring.33 It is important for the multidisciplinary team to agree on risk factor targets, as contrasting advice can confuse and demotivate patients.
Input from an endocrinologist, particularly one who is skilled in the use of insulin pumps, CGM devices and adjunct (off-label) glucose-lowering medications (such as metformin, sodium-glucose cotransporter-2 [SGLT-2] inhibitors or glucagon-like peptide-1 receptor agonists), is essential for optimising glucose control. Most people with type 1 diabetes do not meet the recommended HbA1c targets and pleiotropic effects of adjunct glucose control drugs may also occur. Endocrinologists are often also skilled in more complex BP and lipid care.9,10,34 The REMOVAL trial showed that the use of adjunct metformin retarded atherosclerosis progression in adults with type 1 diabetes and a high CVD risk, and particularly in non-smokers.9,10 The results were based on (surrogate end-point) carotid intima media thickness; however, there are no clinical cardiovascular event outcome data to date.9,10 An endocrinologist can also provide useful input if adjunct drugs such as SGLT-2 inhibitors are needed (e.g. for heart failure).35 They may also assist with treatments or clinical trial access to drugs to retard type 1 diabetes onset and preserve vasoprotective C-peptide for people with recent-onset type 1 diabetes, latent autoimmune diabetes of adults or pre-type 1 diabetes.3
Cardiologist input may also be required to determine the presence of subclinical atherosclerosis and whether medical or surgical intervention is warranted.36-38 Evidence of subclinical disease or novel vascular risk factors, such as high blood levels of lipoprotein(a) (the test for which is not subsidised), may assist in further stratifying risk. Exercise testing (with physical or chemical stressors, and with and without an echocardiography scan) may also be helpful to perform for any patient with type 1 diabetes embarking on an exercise program. If vascular intervention is warranted, the cardiologist can also advise on the merits of open-heart surgery or stenting and the type and duration of antiplatelet therapy. In general, people with type 1 diabetes do better with bypass grafts (preferably arterial rather than venous grafts) than angioplasty.36 Cardiac rehabilitation programs can be useful. Heart failure, including with preserved or reduced ejection fraction, is increasing in people with type 1 diabetes and may be caused by atherosclerosis, hypertension, diabetic cardiomyopathy or valvular disease, or combinations thereof. Heart failure prognosis is worse in type 1 diabetes compared with type 2 diabetes, and there are fewer clinical trial evidence and treatment guidelines for heart failure in type 1 diabetes. A cardiologist can provide advice on heart failure diagnosis, monitoring and treatment.37,38
Conclusion
People with type 1 diabetes experience more aggressive atherosclerosis than those without diabetes. Multiple risk factors are associated with atherosclerosis in people with type 1 diabetes, but ongoing research efforts have resulted in an increasing array of effective therapies. Ongoing patient education and support by a well co-ordinated multidisciplinary team that includes the GP, specialists and allied healthcare professionals is strongly recommended. Additional advocacy for equitable access to useful tests and therapies is needed. ET
COMPETING INTERESTS: Professor Jenkins has received grant funding from Abbot and Medtronic; has received speaker fees for a lecture to the Pharmacist Society; is on the Advisory Boards for Abbott Diabetes Care Division and Insulet Corporation; is the Honourary President for Insulin For Life Global and Australia; and Honourary Chair Elect for the International Diabetes Federation, Western Pacific region. Associate Professor Kilov has received consultation fees from and is on the Advisory Boards for Lilly, Novartis and NovoNordisk; honoraria from Abbott, Astra Zeneca, iNova, InVivo Academy, Lilly, NovoNordisk, REED Medical Education, Roche and Sanofi; and is a Board Member for Insulin For Life. Professor Peter: None.
References
1. National Diabetes Services Scheme (NDSS). Type 1 Diabetes as at 30 June 2022. NDSS; 2022. Available online at: https://www.ndss.com.au/wp-content/uploads/ndss-data-snapshot-202206-type1-diabetes.pdf (accessed October 2023).
2. Jenkins A, Januszewski A, O’Neal D. The early detection of atherosclerosis in type 1 diabetes: why, how and what to do about it. Cardiovasc Endocrinol Meta 2019; 8: 14-27.
3. Vergès B. Cardiovascular disease in type 1 diabetes: a review of epidemiological data and underlying mechanisms. Diabetes Metab 2020; 46: 442-449.
4. Rawshani A, Sattar N, Franzén S, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 2018; 392: 477-486.
5. Chen YC, Jandeleit-Dahm K, Peter K. Sodium-glucose co-transporter 2 (SGLT-2) inhibitor dapagliflozin stabilizes diabetes-induced atherosclerotic plaque instability. J Am Heart Assoc 2022; 11: e022761.
6. Chen YC, Huang AL, Kyaw TS, Bobik A, Peter K. Atherosclerotic plaque rupture: identifying the straw that breaks the camel’s back. Arterioscler Thromb Vasc Biol 2016; 36: e63-e72.
7. Tran-Duy A, Knight J, Clarke PM, Svensson AM, Eliasson B, Palmer AJ. Development of a life expectancy table for individuals with type 1 diabetes. Diabetologia 2021; 64: 2228-2236.
8. Karamanakos G, Kokkinos A, Dalamaga M, Liatis S. Highlighting the role of obesity and insulin resistance in type 1 diabetes and its associated cardiometabolic complications. Curr Obes Rep 2022; 11: 180-202.
9. Petrie JR, Chaturvedi N, Ford I, et al; REMOVAL Study Group. Cardiovascular and metabolic effects of metformin in patients with type 1 diabetes (REMOVAL): a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 2017; 5: 597-609.
10. Timmons JG, Greenlaw N, Boyle JG, et al; REMOVAL Study Group. Metformin and carotid intima-media thickness in never-smokers with type 1 diabetes: the REMOVAL trial. Diabetes Obes Metab 2021; 23: 1371-1378.
11. Ceriello A, Novials A, Ortega E, et al. Evidence that hyperglycemia after recovery from hypoglycemia worsens endothelial function and increases oxidative stress and inflammation in healthy control subjects and subjects with type 1 diabetes. Diabetes 2012; 61: 2993-2997.
12. Kiec-Wilk B, Matejko B, Razny U, et al. Hypoglycemic episodes are associated with inflammatory status in patients with type 1 diabetes mellitus. Atherosclerosis 2016; 251: 334-338.
13. Giménez M, Gilabert R, Monteagudo Jet al. Repeated episodes of hypoglycemia as a potential aggravating factor for preclinical atherosclerosis in subjects with type 1 diabetes. Diabetes Care 2011; 34: 198-203.
14. International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol 2019; 7: 385-396.
15. Wright RJ, Newby DE, Stirling D, Ludlam CA, Macdonald IA, Frier BM. Effects of acute insulin-induced hypoglycemia on indices of inflammation: putative mechanism for aggravating vascular disease in diabetes. Diabetes Care 2010; 33: 1591-1597.
16. Steineck I, Cederholm J, Eliasson B, et al; Swedish National Diabetes Register. Insulin pump therapy, multiple daily injections, and cardiovascular mortality in 18,168 people with type 1 diabetes: observational study. BMJ 2015; 350: h3234.
17. Jenkins AJ, Best JD, Klein RL, Lyons TJ. ‘Lipoproteins, glycoxidation and diabetic angiopathy’. Diabetes Metab Res Rev 2004; 20: 349-368.
18. Chapman MJ. HDL functionality in type 1 and type 2 diabetes: new insights. Curr Opin Endocrinol Diabetes Obes 2022; 29: 112-123.
19. Cholesterol Treatment Trialists’ (CTT) Collaborators; Kearney PM, Blackwell L, Collins R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008; 371: 117-125.
20. Lee P, Jenkins A, Bourke C, et al. Prothrombotic and antithrombotic factors are elevated in patients with type 1 diabetes complicated by microalbuminuria. Diabet Med 1993; 10: 122-128.
21. Kristófi R, Bodegard J, Ritsinger V, et al. Patients with type 1 and type 2 diabetes hospitalized with COVID-19 in comparison with influenza: mortality and cardiorenal complications assessed by nationwide Swedish registry data. Cardiovasc Diabetol 2022; 21: 282.
22. Johansen NJ, Knop FK. The potential of colchicine for lowering the risk of cardiovascular events in type 1 diabetes. Eur Heart J Cardiovasc Pharmacother 2023; 9: 311-317.
23. Bovi TG, Zantut-Wittmann DE, Parisi MCR. Ambivalence about the selection of cardiovascular risk stratification tools: Evidence in a type 1 diabetes population. Diabetes Metab Syndr 2019; 13: 2322-2327.
24. Vistisen D, Andersen GS, Hansen CS, et al. Prediction of first cardiovascular disease event in type 1 diabetes mellitus: the Steno Type 1 Risk Engine. Circulation 2016; 133: 1058-1066.
25. Noriega T, Giménez M, Perea V, et al. Use of the Steno T1 Risk Engine identifies preclinical atherosclerosis better than use of ESC/EASD-2019 in adult subjects with type 1 diabetes at high risk. Diabetes Care 2022; 45: 2412-2421.
26. Rawshani A, Rawshani A, Sattar N, et al. Relative prognostic importance and optimal levels of risk factors for mortality and cardiovascular outcomes in type 1 diabetes mellitus. Circulation 2019; 139: 1900-1912.
27. Hero C, Rawshani A, Svensson AM, et al. Association between use of lipid-lowering therapy and cardiovascular diseases and death in individuals with type 1 diabetes. Diabetes Care 2016; 39: 996-1003.
28. Sivashanmugarajah A, Fulcher J, Sullivan D, Elam M, Jenkins A, Keech A. Suggested clinical approach for the diagnosis and management of ‘statin intolerance’ with an emphasis on muscle-related side-effects. Intern Med J 2019; 49: 1081-1091.
29. Bhatt DL, Steg PG, Miller M, et al; REDUCE-IT Investigators. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med 2019; 380: 11-22.
30. Katsimardou A, Imprialos K, Stavropoulos K, Sachinidis A, Doumas M, Athyros VG. Treatment strategies for hypertension in patients with type 1 diabetes. Expert Opin Pharmacother 2020; 21: 1241-1252.
31. Casu A, Bilal A, Pratley RE; Advancing Care for Type 1 Diabetes, Obesity Network (ACT1ON). Pharmacological therapies to address obesity in type 1 diabetes. Curr Opin Endocrinol Diabetes Obes 2020; 27: 194-206.
32. Dessify B, Wood C, Parker D, Carmichael D, Petrick A, Daouadi M. Is there a role for bariatric surgery in patients with severe obesity and type 1 diabetes? Surg Obes Relat Dis 2022; 18: 177-181.
33. Health Direct. Home Medicine Review. Available online at: https://www.healthdirect.gov.au/home-medicines-review (accessed October 2023).
34. Goyal I, Sattar A, Johnson M, Dandona P. Adjunct therapies in treatment of type 1 diabetes. J Diabetes 2020; 12: 742-753.
35. Primavera M, Giannini C, Chiarelli F. Prediction and prevention of type 1 diabetes. Front Endocrinol (Lausanne) 2020; 11: 248.
36. Domanski MJ, Farkouh ME. Type 1 diabetes, coronary disease complexity, and optimal revascularization strategy. J Am Coll Cardiol 2017; 70: 1452-1454.
37. Gómez-Perez AM, Damas-Fuentes M, Cornejo-Pareja I, Tinahones FJ. Heart failure in type 1 diabetes: a complication of concern? A Narrative Review. J Clin Med 2021; 10: 4497.
38. Shaw JA, Cooper ME. Contemporary management of heart failure in patients with diabetes. Diabetes Care 2020; 43: 2895-2903.