Type 1 diabetes: predicting and achieving long-term survival

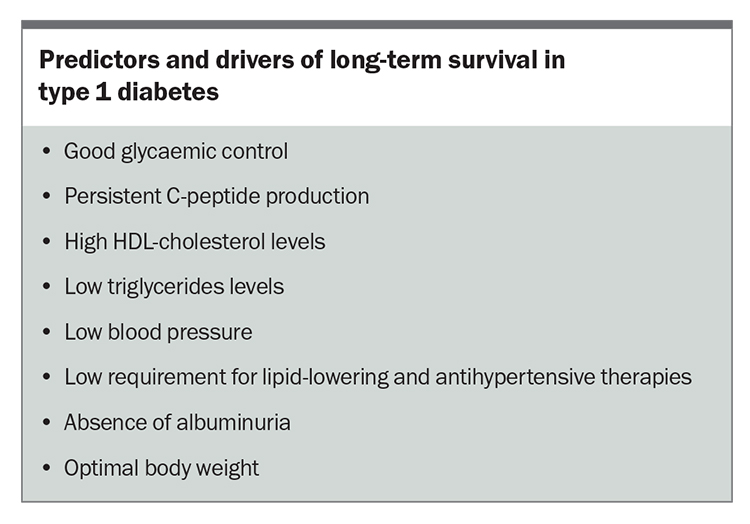
Long-term survival (more than 50 years) without significant complications is well recognised in some people with type 1 diabetes. Most improvements in survival are likely due to effective and careful attention to glycaemic control and management of cardiovascular risk factors and bodyweight.
- It is well recognised that some people with type 1 diabetes are long-term survivors (living with diabetes for 50 years or more) who never develop significant diabetes-related complications.
- Understanding the predictors and drivers of long-term survival helps in the development of new therapies and management strategies for type 1 diabetes.
- Although some people will ‘escape’ complications, most improvements in survival are likely due to effective and careful attention to glycaemic control and management of cardiovascular risk factors and bodyweight.
- Emerging therapies with possible nonglycaemic benefits and strategies that protect and preserve endogenous insulin production have the potential to improve survival in people with type 1 diabetes.
- In the future, new interventions may help to identify both novel markers and mediators to target and prevent diabetes complications.
The discovery of insulin 100 years ago turned the universally fatal type 1 diabetes, that had an average life expectancy of about 3 years, into a chronic and manageable condition.1-3 Survival rates in people with type 1 diabetes are steadily improving, although overall life expectancy remains 10 to 15 years below that of the general population.1,4,5 Chronic complications are, however, not inevitable and some people with type 1 diabetes will live to old-age and never develop a significant diabetes-related complication.4,6
Definitions and challenges of long-term survival studies
Several mostly cohort or cross-sectional studies have assessed specific characteristics of patients reaching extreme diabetes duration milestones.7 No single definition exists, but long-term survival generally refers to living with diabetes for 50 years or more. However, in these studies, duration cut-offs were arbitrary and differentially considered the presence or absence of complications for inclusion. Further, studies of this type are subject to numerous selection biases.7 Despite these challenges, studying people with type 1 diabetes living this long is important for two reasons. First, is to determine if it is possible to predict who is (and perhaps more importantly who is not) going to be a long-term survivor and, second, to identify the possible principal drivers of long-term survival to see if they can be harnessed or modified for every person with type 1 diabetes.
Predictors, determinants and modifiers of long-term survival
Glycaemic control
Glycaemic control is the most important modifiable risk factor associated with risk of complications (see Box). A glycated haemoglobin (HbA1c) level of less than 7% substantially reduces event rates, especially when achieved early and is sustained.2,8 Most, long-term survival studies suggest benefit from lower HbA1c levels. However, in these studies, individual variation was wide and estimates of control over time were limited. For example, in the Joslin 50-Year Medalist Study, patients with type 1 diabetes who survived over 50 years had a mean HbA1c level of 7%, whereas in the UK Golden Years study, it was 7.6% with some participants having HbA1c levels as high as 8.5 to 9% and none having an HbA1c below 7.0%.4,6,9 Further, the role of glucose variability and the impact of advanced technologies to reduce extremes of glucose fluctuation for similar HbA1c levels is still to be determined.
Duration of diabetes
Age of onset or, more specifically, duration of diabetes is a strong predictor of complication development. Interestingly, it is also related to longevity. A diagnosis of type 1 diabetes before the age of 10 years is more likely to be associated with a long-term complication but equally more likely to be associated with surviving more than 50 years compared with a diagnosis after 40 years of age.6 Until recently, age of onset and rate of beta-cell loss were not modifiable risk factors. However, the emergence of new immunotherapies with the potential to slow or delay progression to overt insulin deficiency may substantially affect survival rates 50 years or more later on.10
Persistent C-peptide production
Persistent C-peptide production with less than complete beta-cell loss is associated with better glucose control, reduced glucose variability, less hypoglycaemia, lower risk of complications and
long-term survival. Accurate measures of persistent C-peptide production are challenging, which limits its availability as a predictive tool in routine practice. However, interestingly, the presence of functioning beta cells and preserved insulin secretion in people with type 1 diabetes is far more common than previously thought.7,11 Strategies that protect and preserve beta-cell function are likely to enhance survival and reduce the risk of complications.6
Cardiovascular risk factors
Studies of long-term survival in people with type 1 diabetes have shown inconsistent associations with conventional cardiovascular risk factors. In general, high HDL-cholesterol levels, low blood triglycerides levels, low chronic blood pressure and a low requirement for lipid-lowering and antihypertensive therapies were associated with long-term survival.4,8,12 Similarly, insulin resistance, overweight and lack of physical exercise contribute to future cardiovascular disease and premature mortality, and most long-term survival studies show a positive association with a lean phenotype.6,8 However, specific approaches to nutrition, diet and weight management have not been carefully studied.
Retinopathy
Retinopathy, in some form, will affect more than 90% of people with type 1 diabetes but is not a strong predictor of mortality.4 Cohort studies suggest a greater proportion of long-term survivors do not develop retinal changes, although this could be due to selection bias.
Nephropathy
Nephropathy is a strong predictor of cardiovascular disease and mortality. The incidence of nephropathy peaks about 20 years after the diagnosis of type 1 diabetes but the rate of progression from albuminuria to overt kidney disease decreases with duration of diabetes (to less than 4% per year after 40 years), suggesting the absence of albuminuria or significant progression predicts longer survival.4,6,8,12
Other factors
Lower socioeconomic status, social deprivation and limited access to insulin, modern technologies and multidisciplinary care are all associated with poorer outcomes.1 Few studies have examined psychological characteristics, such as motivation, resilience and comorbid mental health disease in long-term survivors.6 Similarly, genetic influences and the role of emerging noninsulin-based therapies (e.g. sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists) are likely to be important but have not been extensively studied. Emerging molecular pathways and biomarkers, such as retinol binding protein-3 (RBP-3), are also being identified from in vivo and postmortem studies of long-term survivors with type 1 diabetes, which are associated with fewer long-term complications and better survival.13 Understanding and harnessing these factors have the exciting potential for novel interventions to protect against future complications.
Survivors, delayers and escapers
It is likely that long-term survival represents a combination of destiny (at present largely unchangeable factors, such as genetic risk, age of onset, extent of beta-cell damage) and effort (potentially modifiable factors, including glycaemic control, lipid levels, blood pressure, access to care, psychology, motivation, resilience). If so, people with type 1 diabetes could be classified as:
- survivors – those living with significant established complications
- delayers – those destined to develop complications but whose active strategies are effectively delaying their emergence
- escapers – those who are truly destined never to develop complications, irrespective of the management strategies they employ.6
Early survivorship studies erroneously overestimated the protective benefits of surviving the first few decades of diabetes without complications (especially retinopathy and nephropathy).6 It is important to recognise that complications, particularly albuminuria and cardiovascular disease, can emerge after many years of apparent good health and there is risk in the complacency that might come from confusing a delayer with a true escaper.6 Currently, an effective delayer looks very much like a healthy individual without diabetes: lean, fit, resilient and motivated, with longevity genes, excellent glucose control and stability, and persistent endogenous insulin production.6 They also employ effective vascular risk-factor management, use advanced technologies, have excellent health and social supports (and will probably start to incorporate noninsulin-based therapies).
As mentioned earlier, molecular pathways and biomarkers (e.g. RBP-3) from in vivo and postmortem tissue have been identified that are associated with fewer severe diabetes complications, and some of these findings of protection from diabetes-related eye and kidney diseases have been recapitulated in rodent models.13-16 These exciting data suggest that, in the future, new methods to prevent and treat diabetes complications may emerge, for example, expressing RBP-3 into the vitreous and/or retina to protect against vision-threatening retinopathy.13
Conclusion
As clinicians, predicting long-term survival in people with type 1 diabetes is important, as are prospective new interventions. However, for people living with type 1 diabetes, their supporters and carers, aspiring to long-term survival through equitable access to current therapies, healthcare and support and by reducing the burdens of type 1 diabetes is perhaps even more important and are the mainstays of diabetes care. ET
COMPETING INTERESTS: None
References
1. Vanderneit J, Jenkins A, Donaghue K. Epidemiology of type 1 diabetes. Curr Cardiol Reports 2022; 24: 1455-1465.
2. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications of insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 997-986.
3. DCCT/EDIC Research Group. Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care 1999; 22:
99-111.
4. Distiller L. Why do some people with type 1 diabetes live so long? World J Diabetes 2014; 5: 282-287.
5. Gale E. How to survive diabetes. Diabetologia 2009; 52: 559-567.
6. Rawshani A, Sattar N, Franzen S, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 2018; 392: 477-486.
7. Perkins B, Lovblom L, Lanctot S, et al. Discoveries from the study of longstanding type 1 diabetes. Diabetologia 2021; 64: 1189-1200.
8. Miller R, Costacou T. Cardiovascular disease in adults with type 1 diabetes: looking beyond glycaemic control. Curr Cardiol Reports 2022; 24: 1467-1475.
9. Bain B, Gill G, Dyer P, et al. Characteristics of type 1 diabetes of over 50 years duration (the Golden Years Cohort). Diab Med 2003; 20: 808-811.
10. Herald K, Bundy B, Long A, et al. An anti-CD3 antibody, teplizumab, in relatives at risk for type 1 diabetes. New Engl J Med 2019; 381: 603-613.
11. Oram R, Jones A, Besser R, et al. The majority of patients with long duration type 1 diabetes are insulin micro secretors and have functioning beta-cells. Diabetalogia 2014; 57: 187-191.
12. Adamsson Eyrd S, Svensson AM, Franzen S, et al. Risk of future microvascular and macrovascular disease in people with type 1 diabetes of very long duration: a national study with 10-year follow-up. Diabet Med 2017; 34: 411-418.
13. Yokomizo H, Maeda Y, Park K, et al. Retinol binding protein 3 is increased in the retina of patients with diabetes resistant to diabetic retinopathy. Sci Transl Med 2019; 3; 11: eaau6627.
14. Qi W, Keenan HA, Li Q. Pyruvate kinase M2 activation may protect against the progression of diabetic glomerular pathology and mitochondrial dysfunction. Nat Med 2017; 23: 753-762.
15. Fu J, Shinjo T, Li Q, et al. Regeneration of glomerular metabolism and function by podocyte pyruvate kinase M2 in diabetic nephropathy. JCI Insight 2022; 7: e155260.
16. Gordin D, Shah H, Shinjo T, et al. Characterization of glycolytic enzymes and pyruvate kinase m2 in type 1 and 2 diabetic nephropathy. Diabetes Care 2019; 42: 1263-1273.