Bone health during the menopause: assessment and fracture prevention

More than 50% of women over the age of 50 years have osteoporosis or osteopenia. Oestrogen is protective for bones, and rapid bone loss occurs from perimenopause in most women. Optimising bone health during the perimenopause requires an individual assessment of a woman’s risk for fracture, adequate calcium intake, sufficient vitamin D levels and participation in resistance exercise programs. Antiresorptives, osteoanabolic medications or menopausal hormone therapy can also be considered.
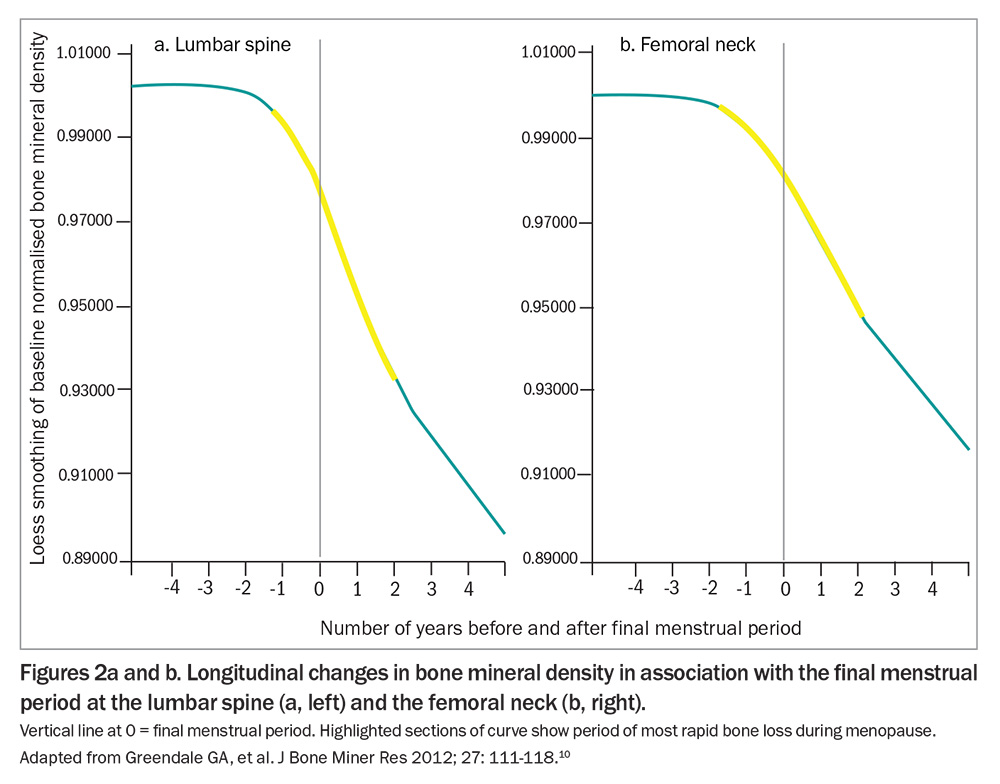
- Bone mineral density declines from perimenopause, with the most rapid loss occurring from one year before to two years following the final menstrual period.
- A diagnosis of osteoporosis should be considered in women with any of the following: a T-score of –2.5 or less at the lumbar spine, hip or radius on dual energy x-ray absorptiometry, a prior minimal trauma fracture or radiological evidence of a vertebral compression fracture (>20% loss of height) without known trauma.
- Fracture Risk Assessment Tool and Garvan Fracture Risk Calculator do not predict osteoporosis development at the time of menopause, and may be less accurate in predicting fracture risk in women during perimenopause.
- Optimising bone health in postmenopausal and perimenopausal women requires adequate dietary calcium intake, sufficient vitamin D levels and participation in high-intensity resistance exercise programs.
- Women with diagnosed osteoporosis should be treated according to local guidelines.
- Menopausal hormone therapy can be considered for bone protection in women not diagnosed with osteoporosis but with a
T-score of –1.8 or less on dual energy x-ray absorptiometry.
One in five women over the age of 50 years have osteoporosis, and over half of the remainder have osteopenia.1 From the age of 50 years, 40% of women will experience an osteoporotic fracture, and 15% will experience a hip fracture.2-4 These fractures lead to pain and loss of mobility, confidence and independence. Following a hip fracture, arguably the most serious consequence of osteoporosis, 20% of people die within 12 months, 20% do not return to their private home (if living independently before the fracture) and only 35% return to their prefracture mobility level by 120 days.5
Pathophysiology
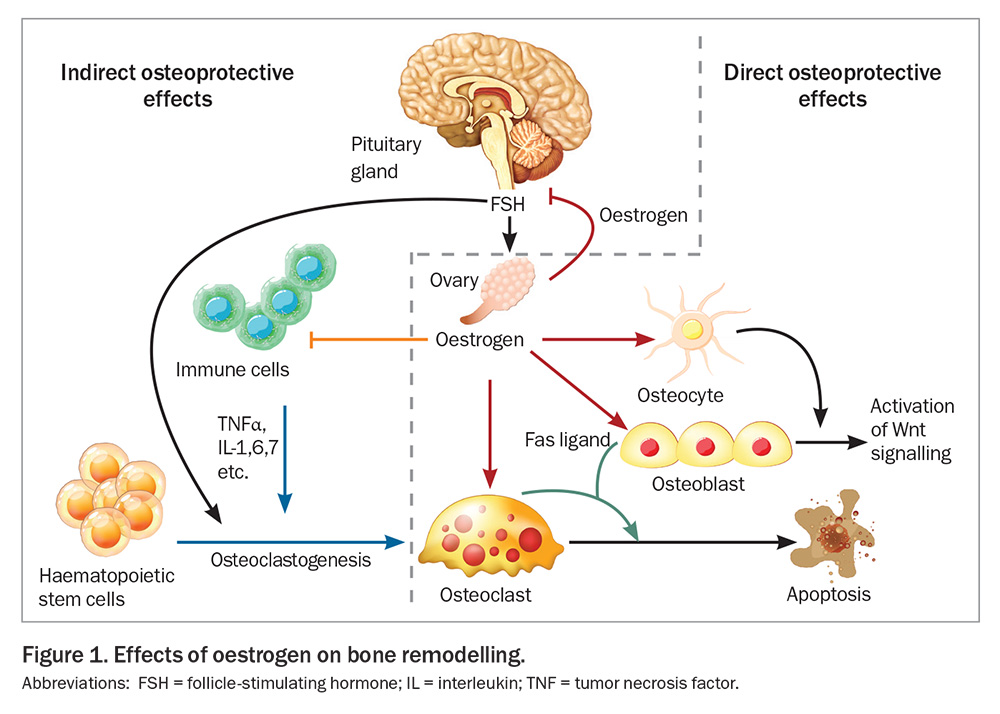
Oestrogen has protective effects on bone. It acts on osteocytes leading to decreased apoptosis and regulation of osteocyte-mediated bone remodelling (the coupling of bone resorption to bone formation). Oestrogen also acts on osteoclasts to reduce bone resorption, acts on osteoblasts to promote bone formation, and lowers renal calcium excretion (Figure 1).6,7 In women, bone accrual occurs during childhood and adolescence, with peak bone mass attained during the third to fourth decade of life, followed by a plateau.8 Bone mineral density (BMD) declines from the perimenopause (where cycle length and menstrual loss begin to vary), with accelerated BMD loss of about 2.5% per year for the first two years postmenopause and then 1% per year for the next three years.9,10 Hence, the most rapid bone loss occurs from one to two years before to two years following the final menstrual period (Figures 2a and b).10
Menopause and its effect on bone loss
Although all women have a decline in BMD during the menopause, the difficulty in management is predicting who will develop osteoporosis and who will fracture. Most fractures in postmenopausal women occur in those who have osteopenia, as defined by dual energy x-ray absorptiometry (DXA) based on T-scores.11 More rapid menopausal bone loss at the spine and a lower baseline lumbar spine BMD at the time of the final menstrual period are associated with a greater risk of fracture.12 However, other predictive factors are less clear. During the perimenopause, low body weight is associated with a greater risk of future osteoporosis and an elevated body mass index is associated with less perimenopausal bone loss; however, fracture rates are similar across body mass index categories.13,14 Women of Asian ethnicity may also have greater bone loss during menopause; however, many studies show their fracture risk is lower than women of European ancestry.10,15
Diagnosis, screening and investigation
DXA is currently the gold standard for the diagnosis of osteoporosis, with osteoporosis defined as a T-score at the lumbar spine, femoral neck, total hip or mid radius of –2.5 or less, and osteopenia defined as a T-score of more than –2.5 and less than –1.0.16 These values relate to postmenopausal women. In practice, osteoporosis should also be diagnosed if there has been a fragility fracture due to minimal trauma (occurring from standing height or less) or there is radiological presence of a vertebral compression fracture (>20% loss of height) without a history of trauma regardless of the T-score.17,18 Nevertheless, in the setting of a known fracture, DXA may be helpful to stratify risk and monitor treatment response but is not essential before initiating specific treatment.
DXA is reimbursed under the Medicare Benefits Schedule (MBS) for people aged 70 years or more, for those with a history of fragility fracture and in those with medical conditions known to decrease BMD (e.g. malabsorptive conditions, chronic kidney or liver diseases, rheumatoid arthritis, thyroxine excess, hyperparathyroidism, hypogonadism or prolonged glucocorticoids).19 In addition to these MBS indications, 2023 Australian menopause guidelines also suggest DXA should be considered in women with normal or low body weight, limited mobility, poor overall health, malnutrition, diabetes mellitus, previous tissue transplant, HIV infection, those who are current smokers and those consuming more than two standard drinks of alcohol per day.20 These indications are not reimbursed under the MBS and so would incur a cost to the patient (from about $105).
In the absence of DXA, readily available online screening tools such as the Fracture Risk Assessment Tool (FRAX; https://frax.shef.ac.uk/FRAX/tool.aspx) and Garvan Fracture Risk Calculator (https://fractureriskcalculator.com.au/calculator/) can provide an estimate of the risk for fracture over the next five to 10 years. However, these tools do not predict osteoporosis development at the time of menopause because they do not take into account the rapid BMD decline that occurs around the final menstrual period. Few studies have examined the use of FRAX in women during perimenopause, and fracture prediction in these women may be less accurate than for older women.21
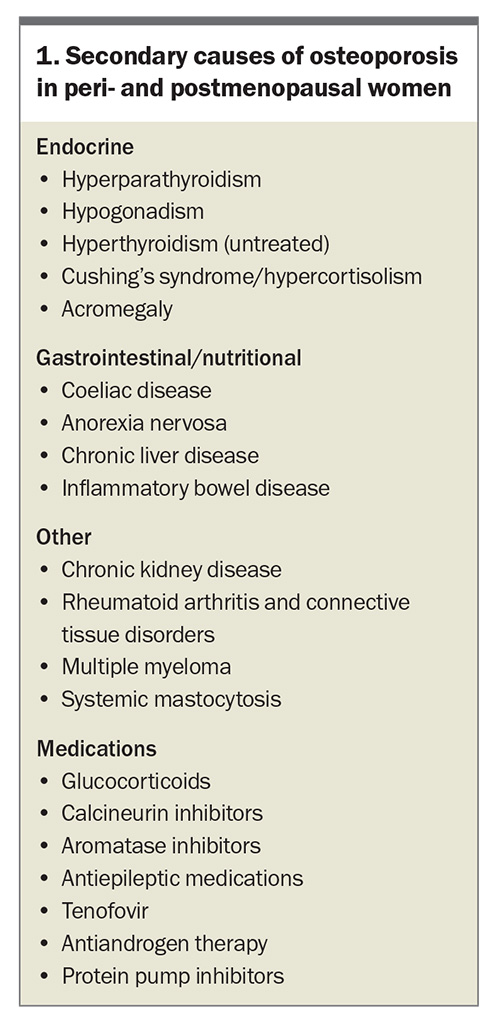
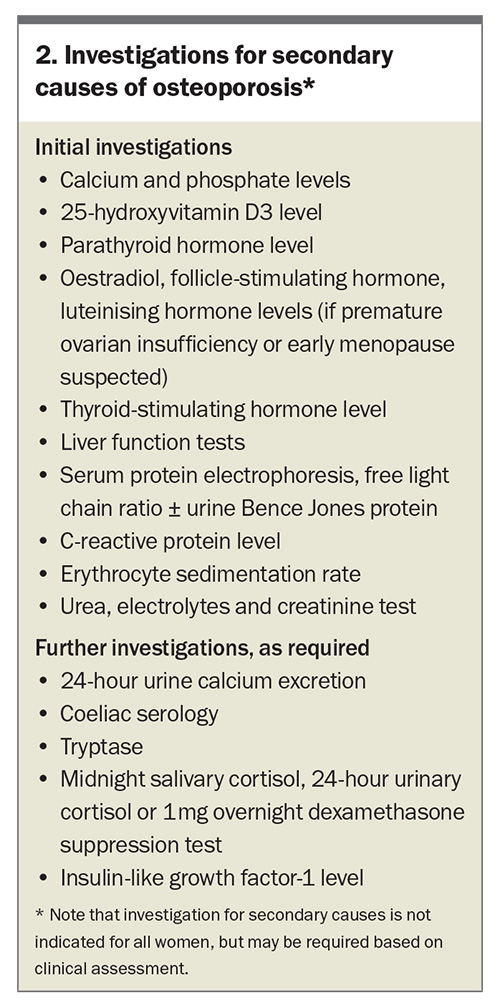
Additional investigations may be required in women diagnosed with osteoporosis. Vitamin D levels should be checked in high-risk women and measurement of renal function and calcium levels are important in treatment selection. Investigations for secondary causes of osteoporosis can be performed if there is clinical suspicion (Box 1 and Box 2).18 Thoraco-lumbar spine x-ray may be performed if vertebral fractures are suspected (kyphosis or ≥3 cm loss of height).
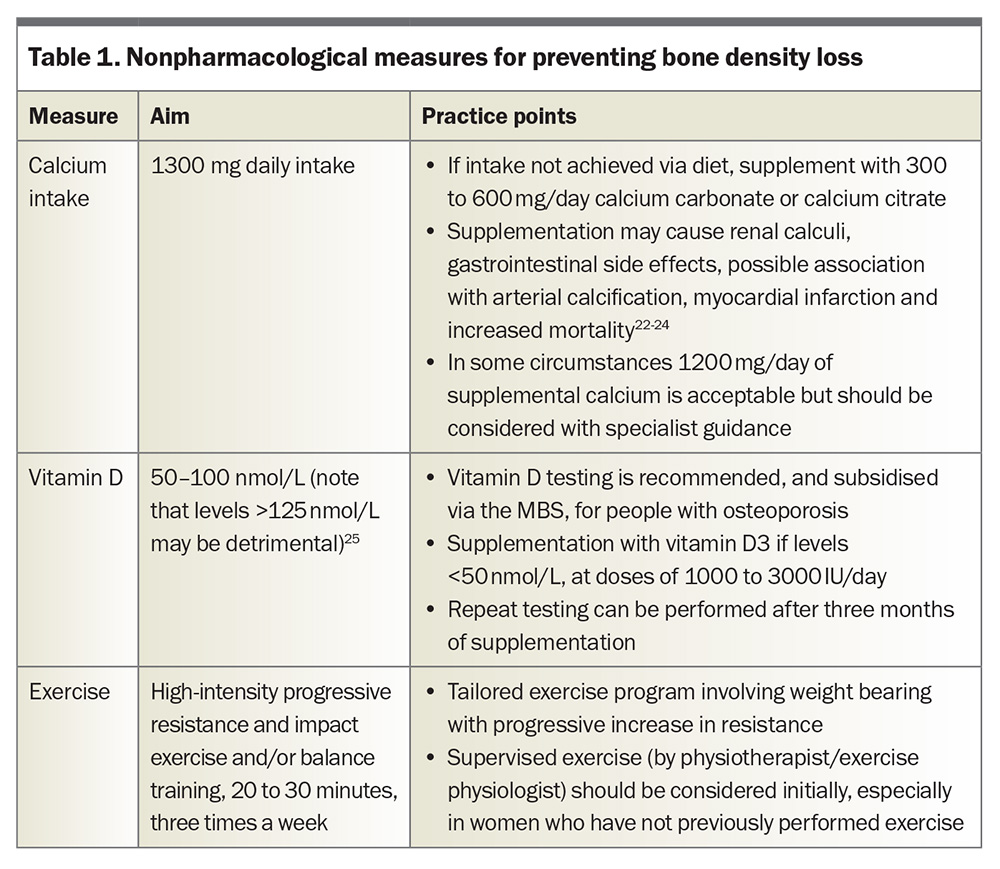
Preventive measures recommended for all women
Conservative measures for preventing bone loss include smoking cessation, minimising alcohol intake (≤10 standard drinks per week and ≤4 standard drinks per day), and ensuring adequate calcium intake and serum vitamin D level. These measures are recommended for all women during the menopause because of their relative safety and the difficulty in predicting who will develop osteoporosis (Table 1).22-25 Australian guidelines recommend 1300 mg daily calcium intake for postmenopausal women, which equates to around three to four servings of dairy (or other calcium-rich food) daily.18,26 Many Australians do not achieve the recommended daily intake, and Healthy Bones Australia (https://healthybones
australia.org.au/) provides factsheets on how this can be achieved, but if this is not possible with diet then a supplement can be considered.27,28
A quarter of Australians are considered vitamin D insufficient (level <50 nmol/L).29 The major source of vitamin D is via sunlight, with only small amounts in the diet. In general, Australians only need to spend a few minutes in sunlight daily over summer to achieve adequate vitamin D levels; however, in winter this may increase to two to three hours per day, and is affected by skin tone and body exposure.28,30 If vitamin D levels are insufficient, vitamin D3 supplements should be started, which are safe and often continued life long.
High-intensity progressive resistance training can increase BMD in pre-, peri- and postmenopausal women, and also may protect against minimal-trauma fractures in postmenopausal women.31-33 In addition, exercise programs and balance training can reduce falls and fall-related fractures.34,35 Specific programs exist around Australia that are tailored for osteoporosis (e.g. Onero – https://onero.academy/osteoporosis-exercises/) and individual programs can also be designed by physiotherapists and excercise physiologists using the Healthy Bones Australia Exercise Prescription Guideline (https://healthybonesaustralia.org.au/wp-content/uploads/2024/02/hba-ex-presc-final-compressed.pdf).
Pharmacological treatment
Women with osteoporosis
Multiple international guidelines recommend using risk-stratification systems to predict the risk of future fractures, and hence the need for pharmacological treatment.17,36,37 A recent fracture is a major risk factor for future fractures; one in 10 people will sustain another fracture within the first 12 months after an initial fracture, and the risk then decreases slowly over time.38,39 In the presence of vertebral or hip fractures, pharmacological therapy is strongly advised. Treatment is also advised in women following other minimal trauma fractures with a T-score of –1.5 or below, and in the absence of a fracture with a T-score of –2.5 or below or a high FRAX score.18 Although some women may not meet PBS criteria for reimbursed antiresorptive agents, the cost of some antiresorptive agents approximates the PBS-reimbursed cost and hence should not be a barrier to warranted pharmacotherapy.
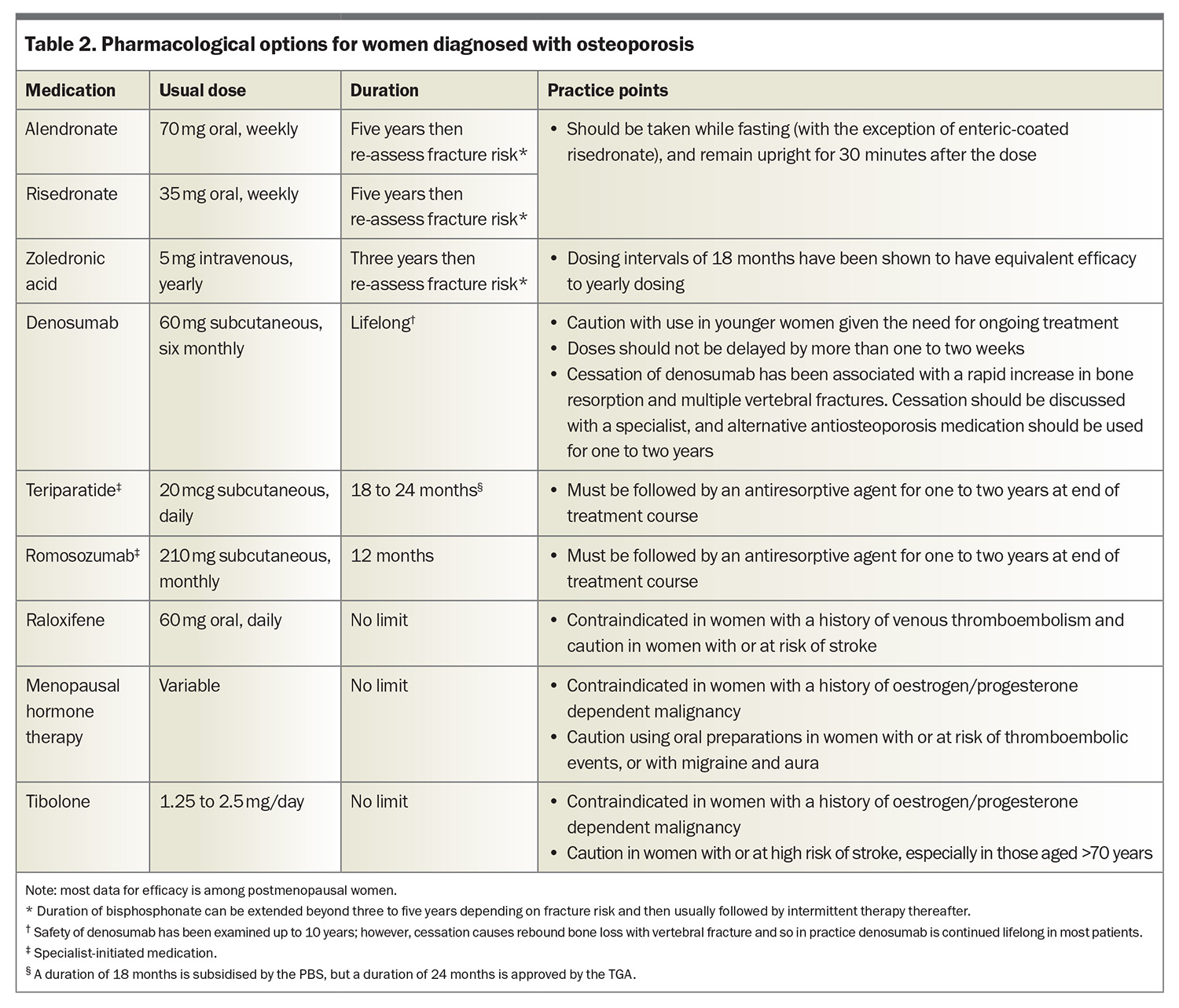
Choice of pharmacotherapy in women with osteoporosis should follow local osteoporosis guidelines.18,40 Options for pharmacological treatment in women with osteoporosis are summarised in Table 2.
Women with osteopenia
In women during the perimenopause and early postmenopause who do not have osteoporosis, consideration may be given to use of menopausal hormone therapy (MHT) to prevent BMD decline, after discussion of the risks versus benefits of therapy. MHT improves BMD at the lumbar spine and to a lesser extent at the hip, and is associated with a 20 to 35% reduction in nonvertebral, vertebral and hip fractures, although the optimal dose for bone preservation is unclear.41-43 In women who have other bothersome symptoms of menopause, MHT is a useful choice for both managing symptoms and providing bone protection. Although there is robust evidence for the use of MHT for bone protection in asymptomatic postmenopausal women with osteopenia, guidelines on who and when to treat have previously been lacking.44 A study examining peripheral BMD in women aged 50 years or above found that those with a T-score of –1.8 or less had increased risk of fractures within the following 12 months.45 Based on this evidence, recent Australian and International menopause guidelines have suggested MHT for asymptomatic women aged under 65 years with a T-score of –1.8 or less (and >–2.5) and a low FRAX risk score, and without contraindications to MHT, to prevent bone loss.20
Alternative options to MHT include low-dose bisphosphonate therapy, which has been shown to improve BMD in early postmenopausal women.46 However, there is a lack of evidence in women commencing treatment around the perimenopause, and this approach is not recommended by current guidelines. Importantly, denosumab is not an appropriate choice for preventive therapy because of the rapid loss of efficacy and rebound increase in bone resorption after cessation.
If or when MHT is stopped, BMD will decline rapidly, with similar rates and magnitude to natural menopause.47 Some studies suggest that fracture incidence following cessation of MHT appears to increase to baseline. In the Women’s Health Initiative trials, rates of fracture following cessation of MHT approximated the placebo group; however, given the reduction in fracture during treatment with MHT, the cumulative fracture prevalence over 13 years was lower in women treated with combined oestrogen and progestogen.48 Importantly, the women in these trials were not all commenced on MHT during the perimenopause, and limited data are available in this age group. A small study examined whether antiresorptive agents can prevent BMD decline after MHT cessation and found that 10 mg alendronate daily for 12 months prevented bone loss and instead led to a rise in BMD at all sites.49 However, this approach has not been incorporated into clinical guidelines.
Monitoring on treatment
If any treatment is commenced, clinical review after three months is appropriate to assess tolerability. A repeat DXA is subsidised under the MBS 12 months after a treatment change or every one to two years depending on the indication. For women who have started treatment, minimal change is expected after 12 months of treatment, and therefore we suggest repeating a DXA only after 24 months in most women, unless there is a clinical suspicion of more rapid BMD change. In women not on treatment, with T-scores less than –2.5, or Z-scores less than 1.5, a repeat DXA is subsidised every two years; in other women, clinicians can consider a privately funded DXA scan to assess the magnitude of perimenopausal bone loss.
Serial DXA should be performed at the same practice, on the same machine to allow for comparison.50 Any difference in BMD on serial DXA should be reported in regard to the least significant change of the machine and operator. If a DXA report states only the percentage change in BMD, with no reference to the significance of this change, or the least significant change of the machine, it is difficult to determine if there has been a true change in BMD or if the difference is simply due to machine variability. In these cases, however, 4 to 5 % in the lumbar spine and 5% elsewhere can be used as a rough estimate of significant change.
Conclusion
Menopause is associated with a significant, rapid decline in BMD, beginning before the final menstrual period. Given the burden of osteoporosis and fractures as women age, identifying women at higher risk, and implementing measures to reduce BMD decline, are vitally important. All women should be encouraged to stop smoking, reduce alcohol intake, optimise calcium intake, have normal vitamin D levels and exercise. Pharmacological options should be considered according to local guidelines, with osteoporosis treatment preferred in women with osteoporosis (fragility fracture and/or a T-score ≤–2.5), and MHT considered in those with T-scores of –1.8 or less. ET
COMPETING INTERESTS: None.
ACKNOWLEDGEMENT: The authors would like to acknowledge Professor Susan Davis for reading an earlier version of this article and providing feedback.
References
1. Henry MJ, Pasco JA, Nicholson GC, Kotowicz MA. Prevalence of osteoporosis in Australian men and women: Geelong Osteoporosis Study. Med J Aust 2011; 195: 321-322.
2. Cooley H, Jones G. A population-based study of fracture incidence in southern Tasmania: lifetime fracture risk and evidence for geographic variations within the same country. Osteoporos Int 2001; 12: 124-130.
3. Doherty DA, Sanders KM, Kotowicz MA, Prince RL. Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int 2001; 12: 16-23.
4. Kanis JA, Norton N, Harvey NC, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 2021; 16: 82.
5. Australian and New Zealand Hip Fracture Registry (ANZHFR). Annual report of hip fracture 2022. Available online at: https://anzhfr.org/wp-content/uploads/sites/1164/2022/08/ANZHFR-2022-Annual-Report-Print-version-v2.pdf (accessed April 2024).
6. Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends Endocrinol Metab 2012; 23: 576-581.
7. Dick IM, Devine A, Beilby J, Prince RL. Effects of endogenous estrogen on renal calcium and phosphate handling in elderly women. Am J Pysiol Endocrinol Metab 2005; 288: E430-E435.
8. Weaver CM, Gordon CM, Janz KF, et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 2016; 27: 1281-386.
9. Ahlborg HG, Johnell O, Turner CH, Rannevik G, Karlsson MK. Bone loss and bone size after menopause. N Engl J Med 2003; 349: 327-334.
10. Greendale GA, Sowers M, Han W, et al. Bone mineral density loss in relation to the final menstrual period in a multiethnic cohort: results from the Study of Women’s Health Across the Nation (SWAN). J Bone Miner Res 2012; 27: 111-118.
11. Pasco JA, Seeman E, Henry MJ, Merriman EN, Nicholson GC, Kotowicz MA. The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int 2006; 17: 1404-1409.
12. Shieh A, Karlamangla AS, Huang MH, Han W, Greendale GA. Faster lumbar spine bone loss in midlife predicts subsequent fracture independent of starting bone mineral density. J Clin Endocrinol Metab 2021; 106: e2491-e501.
13. Zeitlin J, Parides MK, Lane JM, Russell LA, Kunze KN. A clinical prediction model for 10-year risk of self-reported osteoporosis diagnosis in pre- and perimenopausal women. Archives of Osteoporosis 2023; 18: 78.
14. Ishii S, Cauley JA, Greendale GA, et al. Pleiotropic effects of obesity on fracture risk: the Study of Women’s Health Across the Nation. J Bone Miner Res 2014; 29: 2561-2570.
15. Cauley JA, Wu L, Wampler NS, et al. Clinical risk factors for fractures in multi-ethnic women: the Women’s Health Initiative. J Bone Miner Res 2007; 22: 1816-1826.
16. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis : report of a WHO study group. Geneva; 1994.
17. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists / American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis 2020 update. Endocr Pract 2020; 26(Suppl 1): 1-46.
18. Royal Australian College of General Practitioners (RACGP). Healthy Bones Australia. Osteoporosis management and fracture prevention in postmenopausal women and men over 50 years of age. 3nd edn: RACGP; 2024.
19. Australian Government Department of Health and Aged Care. Medicare Benefits Schedule Online: Commonwealth of Australia. Available online at: https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=12312&qt=item (accessed April 2024).
20. Davis SR, Taylor S, Hemachandra C, et al. The 2023 Practitioner’s Toolkit for Managing Menopause. Climacteric 2023; 26: 517-536.
21. Trémollieres FA, Pouillès J-M, Drewniak N, Laparra J, Ribot CA, Dargent-Molina P. Fracture risk prediction using BMD and clinical risk factors in early postmenopausal women: sensitivity of the WHO FRAX tool. J Bone Min Res 2010; 25: 1002-1009.
22. Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev 2014; 2014(4): CD000227.
23. Lewis JR, Radavelli-Bagatini S, Rejnmark L, et al. The effects of calcium supplementation on verified coronary heart disease hospitalization and death in postmenopausal women: a collaborative meta-analysis of randomized controlled trials. J Bone Miner Res 2015; 30: 165-175.
24. Myung SK, Kim HB, Lee YJ, Choi YJ, Oh SW. Calcium supplements and risk of cardiovascular disease: a meta-analysis of clinical trials. Nutrients 2021; 13(2).
25. Ross AC, Manson JE, Abrams SA, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 2011; 96: 53-58.
26. National Health and Medical Research Council. Australian Dietary Guidelines. Canberra: National Health and Medical Research Council; 2013.
27. Australian Bureau of Statistics. Australian Health Survey: Nutrition First Results - Foods and Nutrients Canberra: ABS; 2011. Available online at: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-nutrition-first-results-foods-and-nutrients/latest-release (accessed April 2024).
28. Healthy Bones Australia: Healthy Bones Australia. Available online at: https://healthybonesaustralia.org.au/ (accessed April 2024).
29. Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Nutrients Canberra: ABS; 2011. Available online at: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-biomedical-results-nutrients/2011-12 (accessed April 2024).
30. National Cancer Control Policy contributors. Position statement - Risks and benefits of sun exposure: National Cancer Control Policy; 2018. Available online at: https://wiki.cancer.org.au/policy_mw/index.php?title=Position_statement_-_Risks_and_benefits_of_sun_exposure&oldid=7939 (accessed April 2024).
31. Shojaa M, von Stengel S, Kohl M, Schoene D, Kemmler W. Effects of dynamic resistance exercise on bone mineral density in postmenopausal women: a systematic review and meta-analysis with special emphasis on exercise parameters. Osteoporos Int 2020; 31: 1427-1444.
32. Hoffmann I, Kohl M, von Stengel S, et al. Exercise and the prevention of major osteoporotic fractures in adults: a systematic review and meta-analysis with special emphasis on intensity progression and study duration. Osteoporos Int 2023; 34: 15-28.
33. Sañudo B, de Hoyo M, del Pozo-Cruz J, et al. A systematic review of the exercise effect on bone health: the importance of assessing mechanical loading in perimenopausal and postmenopausal women. Menopause 2017; 24: 1208-1216.
34. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 2012(9): CD007146.
35. El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 2013; 347: f6234.
36. Shoback D, Rosen CJ, Black DM, Cheung AM, Murad MH, Eastell R. Pharmacological management of osteoporosis in postmenopausal women: an endocrine society guideline update. J Clin Endocrinol Metab 2020; 105(3): dgaa048.
37. Kanis JA, Harvey NC, McCloskey E, et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 2020; 31(1): 1-12.
38. Balasubramanian A, Zhang J, Chen L, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 2019; 30: 79-92.
39. Hansen D, Pelizzari P, Pyenson B. Medicare cost of osteoporotic fractures - 2021 updated report. The clinical and cost burden of fractures associated with osteoporosis. Milliman Research Report For the National Osteoporosis Foundation; 2021.
40. Ebeling PR, Seeman E, Center J, et al. Position Statement on the Management of Osteoporosis: Healthy Bones Australia; 2022 https://healthybonesaustralia.org.au/wp-content/uploads/2023/01/position-statement-on-osteoporosis-dec-2022.pdf (accessed May 2024).
41. Wells G, Tugwell P, Shea B, et al. Meta-analysis of the efficacy of hormone replacement therapy in treating and preventing osteoporosis in postmenopausal women. Endocrine Reviews 2002; 23: 529-539.
42. Barrionuevo P, Kapoor E, Asi N, et al. Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: a network meta-analysis. J Clin Endocrinol Metab 2019; 104: 1623-1630.
43. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women principal results from the women’s health initiative randomized controlled trial. JAMA 2002; 288: 321-333.
44. The North American Menopause Society. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause 2022; 29: 767-794.
45. Miller PD, Barlas S, Brenneman SK, et al. An approach to identifying osteopenic women at increased short-term risk of fracture. Arch Intern Med 2004; 164: 1113-1120.
46. Hosking D, Chilvers Clair ED, et al. Prevention of bone loss with alendronate in postmenopausal women under 60 years of age. N Engl J Med 1998; 338: 485-492.
47. Wasnich RD, Bagger YZ, Hosking DJ, et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause 2004; 11(6 Part 1 of 2).
48. Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA 2013; 310: 1353-1368.
49. Ascott-Evans BH, Guanabens N, Kivinen S, et al. Alendronate prevents loss of bone density associated with discontinuation of hormone replacement therapy: a randomized controlled trial. Arch Intern Med 2003; 163: 789-794.
50. The International Society for Clinical Densitometry. 2019 ISCD official positions - adult 2019. Available online at: https://www.iscd.org/official-positions/2019-iscd-official-positions-adult/ (accessed April 2024).