Pregnancy planning for women with type 2 diabetes

Type 2 diabetes is becoming more prevalent in young adults, and GPs have an increasingly important role in identifying and counselling women with diabetes who may become pregnant. It is important to optimise management of the condition before pregnancy to reduce the risk of diabetes-related complications in mothers and their children.
- Type 2 diabetes in pregnancy carries an increased risk of adverse fetal and maternal outcomes, and this risk rises with higher glycated haemoglobin (HbA1c) levels.
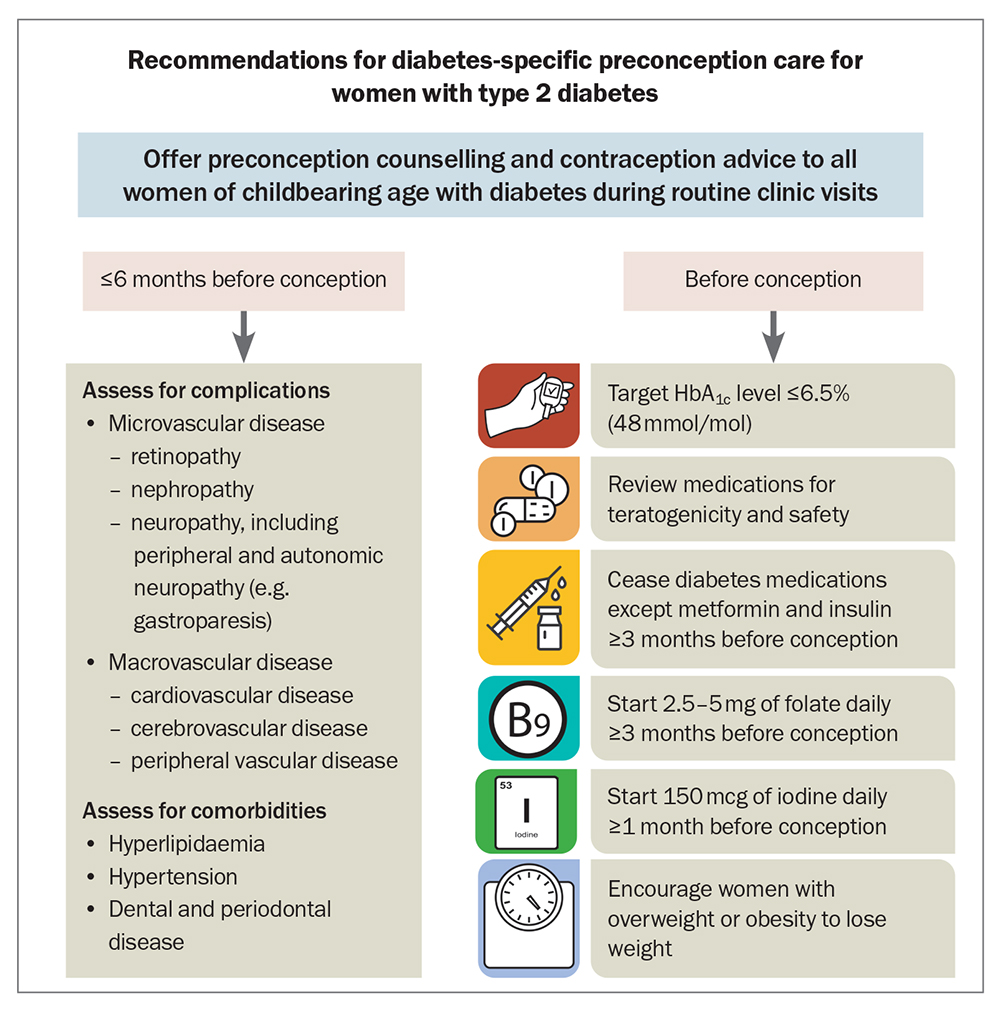
- Preconception care for women with type 2 diabetes should include counselling and education about risks, contraception and pregnancy planning, glycaemic targets, medications, insulin management, complications and weight.
- Before pregnancy, an HbA1c target of less than or equal to 6.5% (48mmol/mol) is recommended; until this target is achieved, women should be offered long-acting, reversible contraception to prevent unplanned pregnancy and complications.
- Assessment of diabetes-related complications and comorbidities should ideally occur within six months before pregnancy.
- All glucose-lowering therapies, apart from metformin and insulin, should be ceased in preparation for conception.
- For women with a body mass index in the overweight or obese range, weight loss should be encouraged before pregnancy to reduce the risk of fetal and maternal complications.
With the rising prevalence of type 2 diabetes in young adults in Australia, the number of pregnancies in women with pre-existing type 2 diabetes is also rising.1 Diabetes increases the risk of maternal and fetal adverse events, which are mainly attributable to hyperglycaemia. This risk increases with higher glycated haemoglobin (HbA1c) levels during periconception and pregnancy. It is not uncommon for type 2 diabetes to be first diagnosed during pregnancy itself, and GPs play a key role in identifying and counselling women with diabetes both before and throughout their pregnancy.
Early detection of diabetes and initiation of management are vital to enable risk factor modification and encouragement of a healthy lifestyle, to reduce the adverse effects of type 2 diabetes on women and their children. This article reviews the recommended preconception care and counselling for women with pre-existing type 2 diabetes, as well as management of diabetes during pregnancy.
Risks of type 2 diabetes in pregnancy
Observational studies have found an increased risk of diabetic embryopathy with elevations of HbA1c levels in the first 10 weeks of pregnancy.2 This includes congenital heart disease, anencephaly, microcephaly, renal anomalies and caudal regression syndrome. The most common of these complications are cardiovascular defects, including atrioventricular septal defects, transposition of great arteries and tricuspid atresia. The risk of congenital anomalies increases with deteriorating glycaemic control, with a threefold rise when HbA1c is greater than or equal to 6.2% (44 mmol/mol), and a more than sixfold rise once HbA1c is 8.5% (69 mmol/mol) or higher.2 The risk of caudal regression syndrome (a devastating malformation that can manifest as lumbosacral agenesis with renal and anogenital anomalies and fusion of the lower extremities) in children born to women with type 2 diabetes is one in 350 births, which is about 200 times the rate seen in the general population.3 Other risks associated with hyperglycaemia in pregnancy include increased rates of miscarriage, pre-eclampsia, macrosomia, intrauterine growth restriction and new-onset or deterioration of existing diabetes-related complications, especially retinopathy.
A study of 180 Australian women with type 1 or type 2 diabetes found a perinatal mortality rate of 3.4%, compared with 0.7% in the general population. Five of the six perinatal deaths were children of women with type 2 diabetes. The rate of congenital anomalies was 10% in children of women with type 2 diabetes, compared with 6% for children of women with type 1 diabetes and 2.1% in the general population.4 A case-control study found that mothers with type 2 diabetes experience higher rates of gestational hypertension, elective caesarean delivery, neonatal hypoglycaemia and neonatal intensive care admission than women with type 1 diabetes.5
A more recent study investigated outcomes for pregnant women with type 1 or type 2 diabetes using a dataset of more than 15,000 pregnancies.6 For women with type 2 diabetes, the rate of preterm delivery was 23.4%, the rate of babies being born large for gestational age was 26.2% and the rate of congenital anomaly was 4.1%. The rate of neonatal death was higher among babies of women with type 2 diabetes than babies of women with type 1 diabetes. Independent risk factors for perinatal death, including stillbirth or neonatal death, included a third-trimester HbA1c level greater than or equal to 6.5% (48 mmol/mol) and having type 2 diabetes.6
The strongest predictors of diabetes-related adverse outcomes are poor glycaemic control, elevated body mass index (BMI) and pre-existing hypertension or nephropathy.7 The Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study observed 260 women with pregestational type 2 diabetes (diagnosed in youth or young adulthood) and with demonstrated socioeconomic disadvantage, high BMI, suboptimal glycaemic control and very low rates of preconception counselling and contraception use.8 Rates of maternal hypertension, preterm birth and stillbirth in this high-risk cohort were triple those in the general population.
Preconception counselling and care
For women with type 2 diabetes, preconception care should include counselling and education about risks, contraception and pregnancy planning, glycaemic targets, medications and insulin management, along with complications, weight assessment and lifestyle management. Primary care providers should be opportunistic and incorporate a question about a woman’s plans for pregnancy into routine assessment and care. This should be revisited regularly during clinical visits because of the risk of unplanned pregnancy.
Care of women with diabetes who are or are planning to become pregnant should ideally be delivered by a multidisciplinary team, including an endocrinologist, a maternal-fetal medicine specialist, a dietitian and a diabetes educator. Through a focus on improving glycaemic management, multidisciplinary team management during preconception and pregnancy has been shown to improve diabetes and pregnancy outcomes.9 For women living in rural or remote Australia, primary care providers should enquire about shared care with major institutions via telehealth.
A summary of the recommendations for diabetes-specific preconception care for women with type 2 diabetes is shown in the Figure.
Contraception and pregnancy planning
Until glycaemic targets are achieved, women should be offered options for long-acting, reversible contraception, such as hormonal and nonhormonal intrauterine contraceptive devices and subcutaneous progestogen implants, to prevent unplanned pregnancy.10 The oral contraceptive pill or barrier contraceptive methods can be used if this is a woman’s preference, but long-acting methods are preferable to reduce the risk of unplanned pregnancy.
The use of preconception counselling using educational tools has been shown to help teenage girls make well-informed decisions.11 Such tools include the National Diabetes Services Scheme (NDSS) pregnancy planning checklist and an NDSS resource on contraception choices for women with diabetes.12,13 The 2020 Australasian Diabetes in Pregnancy Society (ADIPS) guideline on pre-existing diabetes in pregnancy provides detailed recommendations for healthcare providers.14
Glycaemic targets
All women of reproductive age with type 2 diabetes should be counselled on the importance of achieving and maintaining euglycaemia before conception and throughout pregnancy. Blood glucose levels (BGLs) should be strictly monitored.
Before pregnancy, an HbA1c target of less than or equal to 6.5% (48 mmol/mol) is recommended, as it is associated with the lowest risk of congenital anomalies, while minimising the risk of hypoglycaemia.2,15 For women with pre-existing type 2 diabetes who are planning pregnancy, ADIPS recommends a fasting and premeal BGL target of less than 6.0 mmol/L and targets of less than 8.5 mmol/L one hour after a meal or less than 7.5 mmol/L two hours after a meal.13
During pregnancy, women are most insulin sensitive between six and 10 weeks’ gestation. Beyond 10 weeks’ gestation, insulin resistance rises. As plasma volume expansion leads to relative dilution of maternal BGLs, the HbA1c target tightens to 6% or lower (42 mmol/mol) by mid-pregnancy.15 For women with pre-existing type 2 diabetes, ADIPS recommends a fasting and premeal BGL target during pregnancy of 4.0 to 5.3 mmol/L and targets of 5.5 to 7.8 mmol/L one hour after a meal or 5.0 to 6.7 mmol/L two hvours after a meal.13
Medication review
Women’s medication lists should be reviewed for potential teratogenic agents. All glucose-lowering therapies, apart from metformin and insulin, should be ceased in preparation for conception. If pregnancy occurs unexpectedly and the patient is taking metformin or a sulfonylurea, these agents should be continued initially until endocrinology review, to mitigate the risk of a sudden deterioration in BGLs. Other agents, including glucagon-like peptide 1 receptor agonists, sodium glucose cotransporter 2 inhibitors, thiazolidinediones and dipeptidyl-peptidase 4 inhibitors, should be discontinued immediately, given the limited safety data on their use in pregnancy.10 Ideally, they should be ceased at least three months before planned conception.
Close attention should also be paid to medications prescribed for the management of type 2 diabetes-related complications, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs) and statins, as they are potentially harmful.16,17 Antihypertensive agents that are considered safe in pregnancy include labetalol, methyldopa, nifedipine and hydralazine. However, if an ACE inhibitor or ARB is being used for nephroprotection, it should be continued until a positive pregnancy test result is obtained, as the benefit is deemed to outweigh the risk in this setting.
In addition, it is recommended that all women with type 2 diabetes start taking 5 mg of folic acid daily (or 2.5 mg daily if also taking another folate-containing supplement) at least three months before conception, and continue this throughout the first trimester, to reduce the risk of neural tube defects.18 Iodine supplementation of 150 mcg daily should begin at least one month before conception and continue throughout pregnancy and breastfeeding. At 10 to 12 weeks’ gestation, women should start taking 100 to 150 mg of aspirin nightly, and continue this until 36 weeks’ gestation, to reduce the risk of early-onset pre-eclampsia.13,19
Approach to insulin management
Insulin is the standard of care for managing diabetes in preconception and pregnancy, preferably through an individualised basal bolus regimen with insulin isophane and insulin aspart or lispro.20 If the patient is already being treated with insulin, doses should be adjusted to achieve the glycaemic targets above. If insulin initiation is required, it should ideally be started about three months before conception (once other medications are ceased) to allow for adequate titration. There are several methods for initiating insulin, and national guidelines lack an algorithm to guide dosing initiation and titration. Titration should ideally occur under the guidance of diabetes health professionals with expertise in the care of women with diabetes during pregnancy.
If fasting BGLs are above the target specified above, nightly (before bed) isophane insulin should be started, usually with an initial dose of 8 to 15 units. Rapid-acting insulin should be used before whichever meals tend to be associated with elevated postprandial BGLs, usually with initial doses of 4 to 8 units administered 15 to 20 minutes before the meal. Insulin doses should then be titrated every three to seven days initially and every one to two weeks thereafter throughout the pregnancy to achieve optimal glycaemia.
Assessment for complications and comorbidities
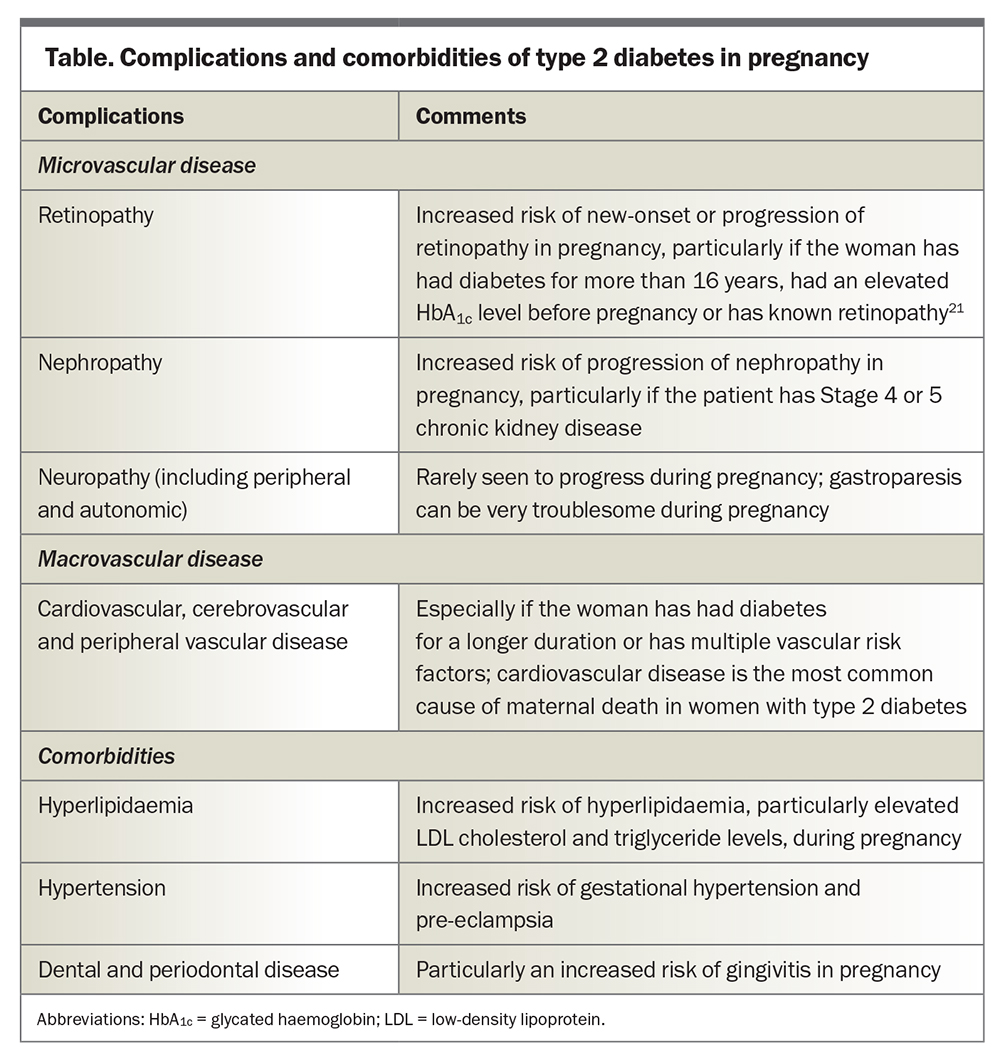
Assessment of diabetes-related complications and comorbidities should ideally occur within six months before pregnancy. This includes assessment for microvascular disease, macrovascular disease and diabetes-related comorbidities (Table).
Weight and lifestyle management
Obesity is a major driver of type 2 diabetes and is an independent contributor to maternal and fetal complications in pregnancy, including congenital anomalies, macrosomia and preterm birth. It has been shown that weight loss before conception reduces the incidence of these complications.22 Therefore, women with a BMI in the overweight or obese range should be encouraged to lose weight before pregnancy. In women of European descent, the overweight BMI range is 25 to 29.9 kg/m2 and the obese range is 30 kg/m2 or higher, while in Asian women these ranges are 23 to 27.4 kg/m2 and 27.5 kg/m2 or higher, respectively.
Weight loss can be pursued through structured diet and exercise programs. Glucagon-like peptide 1 receptor agonists can also be considered but should always be prescribed alongside contraception, given their reproductive toxicity (Category D), and ceased at least three months before planned conception.
Bariatric surgery should be considered if these measures are not successful in women with obesity. No randomised controlled trials have evaluated maternal and fetal outcomes of pregnancy after bariatric surgery in women with type 2 diabetes. Ideally, women should wait at least 12 months after bariatric surgery before falling pregnant, to avoid fetal exposure to the impact of rapid maternal weight loss and to minimise surgical complications during pregnancy. In addition, women should be monitored for micronutrient and macronutrient deficiencies after having bariatric surgery, particularly after gastric bypass surgery, and all need lifelong multivitamin supplementation, with additional micronutrients as individually indicated.23
Other lifestyle management measures include counselling about maintaining a healthy balanced diet, remaining physically active and quitting smoking.
Conclusion
The prevalence of type 2 diabetes in young women is rising and, as a consequence, so is its prevalence in pregnant women. Provision of preconception counselling and care through a multidisciplinary team is essential to achieve euglycaemia and initiate appropriate management before conception and therefore to mitigate maternal and fetal risks of type 2 diabetes in pregnancy. In reality, not all pregnancies are planned. For women with pre-existing diabetes and an unplanned pregnancy, the same principles apply. Strategies are needed to improve screening and diagnosis of type 2 diabetes in young women, to allow for optimal maternal and neonatal outcomes and to reduce unplanned pregnancies by improving contraception uptake. ET
COMPETING INTERESTS: None.
References
1. Temple R, Murphy H. Type 2 diabetes in pregnancy – an increasing problem. Best Pract Res Clin Endocrinol Metab 2010; 24: 591-603.
2. GuerinA, NisenbaumR, RayJG. Use of maternal GHb concentration to estimate the risk of congenital anomalies in the offspring of women with prepregnancy diabetes. Diabetes Care2007; 30: 1920-1925.
3. Mills JL. Malformations in infants of diabetic mothers. Teratology 25:385-94. 1982. Birth Defects Res A Clin Mol Teratol 2010; 88: 769-778.
4. McElduff A, Ross GP, Lagstrom JA, et al. Pregestational diabetes and pregnancy: an Australian experience. Diabetes Care 2005; 28: 1260-1261.
5. Owens LA, Sedar J, Carmody L, Dunne FJ. Comparing type 1 and type 2 diabetes in pregnancy– similar conditions or is a separate approach required? BMC Pregnancy Childbirth 2015; 15: 69.
6. Murphy HR, Howgate C, O’Keefe J, et al; National Pregnancy in Diabetes (NPID) advisory group. Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: a 5-year national population-based cohort study. Lancet Diabetes Endocrinol 2021; 9: 153-164.
7. Handisurya A, Bancher-Todesca D, Schober E, et al. Risk factor profile and pregnancy outcome in women with type 1 and type 2 diabetes mellitus. J Womens Health (Larchmt) 2011; 20: 263-271.
8. TODAY Study Group. Pregnancy outcomes in young women with youth-onset type 2 diabetes followed in the TODAY study. Diabetes Care 2022; 45: 1038-1045.
9. MurphyHR, RolandJM, SkinnerTC, et al. Effectiveness of a regional prepregnancy care program in women with type 1 and type 2 diabetes: benefits beyond glycemic control. Diabetes Care2010; 33: 2514-2520.
10. Wong J, Ross GP, Zoungas S, et al. Management of type 2 diabetes in young adults aged 18–30 years: ADS/ADEA/APEG consensus statement. Med J Aust 2022; 216: 422-429.
11. Charron-ProchownikD, SereikaSM, BeckerD, et al. Long-term effects of the booster-enhanced READY-Girls preconception counseling program on intentions and behaviors for family planning in teens with diabetes. Diabetes Care2013; 36: 3870-3874.
12. Pregnancy planning checklist. National Diabetes Services Scheme; 2020. Available online at: https://www.ndss.com.au/about-diabetes/pregnancy/pregnancy-planning-checklist/ (accessed July 2023).
13. Contraception choices for women with diabetes. National Diabetes Services Scheme; 2023. Available online at: https://www.ndss.com.au/living-with-diabetes/everyday-life-with-diabetes/sexual-health/contraception/ (accessed July 2023).
14. Rudland VL, Price SAL, Hughes R, et al. ADIPS 2020 guideline for pre-existing diabetes and pregnancy. Aust N Z J Obstet Gynaecol 2020; 60: E18-E52.
15. Alexopoulos AS, Blair R, Peters AL. Management of preexisting diabetes in pregnancy: a review. JAMA 2019; 321: 1811-1819.
16. BulloM, TschumiS, BucherBS, BianchettiMG, SimonettiGD. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension2012; 60: 444-450.
17. BatemanBT, Hernandez-DiazS, FischerMA, et al. Statins and congenital malformations: cohort study. BMJ2015; 350: h1035.
18. AlexanderEK, PearceEN, BrentGA, et al. 2017 guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid2017; 27: 315-389.
19. National Institute for Health and Care Excellence. Hypertension in pregnancy: quality standard. Manchester: NICE; 2013 (last updated 23 July 2019). Available online at: https://www.nice.org.uk/guidance/qs35/resources/hypertension-in-pregnancy-2098607923141 (accessed July 2023).
20. Blum AK. Insulin use in pregnancy: an update. Diabetes Spectr 2016; 29: 92-97. Erratum in: Diabetes Spectr 2016; 29: 191.
21. ChewEY, MillsJL, MetzgerBE, et al; National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Metabolic control and progression of retinopathy: the Diabetes in Early Pregnancy Study. Diabetes Care1995; 18: 631-637.
22. Price SAL, Sumithran P, Nankervis AJ, Permezel M, Prendergast LA, Proietto J. Impact of preconception weight loss on fasting glucose and pregnancy outcomes in women with obesity: a randomized trial. Obesity (Silver Spring) 2021; 29: 1445-1457.
23. Monson M, Jackson M. Pregnancy after bariatric surgery. Clin Obstet Gynecol 2016; 59: 158-171.