A 49-year-old woman with perimenopausal symptoms
This case study describes a 49-year-old woman who presents with irregular and heavy periods, disturbed sleep and increasing anxiety and stress levels. Lifestyle recommendations, treatments options to manage heavy and irregular periods and her contraceptive needs are discussed.
- Management of women with perimenopausal symptoms should start with lifestyle recommendations.
- Prescribing oestradiol-containing combined oral contraceptive pill in the perimenopause can help treat heavy and/or irregular periods, provide contraception and relieve hot flushes and sweats.
- Although the levonorgestrel-releasing intrauterine device provides effective contraception and reduces menstrual bleeding over time, it has no effect on vasomotor symptoms, and additional oestrogen is required with its use, usually as an oestradiol patch or gel.
- It is important to tailor the therapy to meet each individual woman’s needs.
Perimenopause is defined from the onset of irregular periods until 12 months after the final menstrual period, specifically with at least a seven-day difference between cycle lengths.1 Towards the end of the reproductive years, fertility diminishes and ovarian activity becomes erratic, leading to potential menstrual irregularity and the development of symptoms representing both low and high hormonal levels. Anovulatory cycles (i.e. absence of ovulation) become more frequent and can lead to irregular periods, increasing the risk of endometrial proliferation, hyperplasia and possible endometrial cancer. Ovulation may occur twice in a menstrual cycle, the second time being during a period known as luteal out of phase ovulation.2
For many women, the perimenopause is a time of change in wellbeing, mood and coping capacity as well as menstrual irregularity and physical symptoms. Some women will experience increasing premenstrual symptoms, heavy and/or erratic periods and abnormal bleeding. Oestrogen levels at this time may be quite high, and may cause breast tenderness, bloating, anxiety or headaches.2 Women may also have low oestrogen levels, leading to vasomotor symptoms, including night sweats and flushes that are intermittent or regular.
Case scenario
Ms A is a 49-year-old secondary school teacher who is divorced with two adult children aged 21 and 23 years. She has experienced irregular periods for eight months and had a recent heavy period with clots lasting 10 days after two months of amenorrhoea. She has increasing anxiety and stress levels, with less capacity to manage her life. Her sleep pattern is disturbed; she is waking up at night feeling hotter than normal and is tired.
She has a new partner and is concerned about using appropriate contraception. Her general health is good, she exercises regularly, has a good diet and is not on any medications, except for vitamin D 1000 IU per day. She is a nonsmoker and drinks alcohol rarely. There is no significant medical or surgical history except for the delivery of her two children by caesarean section. Her mother had morbid obesity and severe hypertension, and died at the age of 78 years of a heart attack. Her father is 82 years old and has type 2 diabetes, but is otherwise well.
General and gynaecological examination reveals her uterus is bulky, similar in size to a nine-week pregnancy.
Assessment
The first steps are assessing Ms A and determining the differential diagnoses. The following issues should be considered with regard to Ms A’s symptoms, history and examination:
- irregular periods
- heavy menstrual bleeding (HMB)
- wakefulness
- anxiety and stress
- increased body heat
- new relationship
- contraception
- bulky uterus.
Based on Ms A’s symptoms and history, a number of differential diagnoses should be considered.
- Perimenopause – her age and the symptom complex are consistent with the perimenopause.
- Endometrial hyperplasia – HMB with clots after a few months of amenorrhoea may be associated with a thickened endometrium. Also, anovulatory cycles during the perimenopause lead to endometrial proliferation and thickening. This is of more concern in women with obesity, as testosterone is metabolised to oestrogen in peripheral fat leading to added oestrogen stimulation.
- Adenomyosis or fibroids – both can cause a bulky uterus and HMB.
- Spontaneous abortion/miscarriage – she experienced HMB after a period of amenorrhoea. She is also concerned about contraception.
- Sleep disorder – she is wakeful and tired.
- Anxiety disorder – mood disorders are common or recur in women in their 40s and 50s due to changing hormone levels.
- Thyroid dysfunction – may develop around the perimenopausal period.
- Diabetes – may cause flushing.
Investigations
Given the above differential diagnoses, the following investigations should be carried out:
- full blood examination
- pregnancy test
- thyroid function test
- iron studies
- fasting blood glucose level
- ultrasound transvaginal (preferably when the period is ceasing or immediately after, as the endometrium will be at its thinnest).
Hormone level tests are not routinely recommended in the perimenopause because they are very variable at this time and unlikely to assist in the diagnosis. For instance, it is possible to see oestradiol levels suggestive of ovulation one week and elevated follicle stimulating hormone level the next. Occasionally, when there are no discernible cycles or a woman has had a hysterectomy, a series of hormone level tests may be required. If a diagnosis is made on a single hormone level in the perimenopause, inappropriate treatment may be prescribed.
Management
Ms A’s management should start with lifestyle recommendations, including:
- eating nutritious foods
- maintaining a regular exercise program
- having regular routine screening and medical examinations, including blood pressure and breast examinations
- having a cervical screen test
- having regular mammograms
- having regular screening for cardiovascular disease and bone health.
Perimenopausal irregular bleeding is common but an assessment of the endometrial thickness on ultrasound is important to determine whether Ms A requires an endometrial biopsy or hysteroscopy and curettage to exclude endometrial hyperplasia or carcinoma. There are a number of treatment options to manage both her irregular heavy periods and her contraceptive needs. These include the combined oral contraceptive pill or ring, the levonorgestrel-releasing intrauterine device and the 4 mg drospirenone pill. Stabilising her cycle and providing contraception may help to relieve Ms A’s anxiety and stress. Prescribing oestradiol-containing combined oral contraceptive in the perimenopause can help treat heavy and/or irregular periods, provide contraception and relieve hot flushes and sweats. They also have lesser effects on haemostasis, fibrinolysis markers, lipids and carbohydrate metabolism.3 Although the levonorgestrel-releasing intrauterine device provides effective contraception and reduces menstrual bleeding over time, it has no effect on vasomotor symptoms, and additional oestrogen is required with its use, usually as an oestradiol patch or gel.
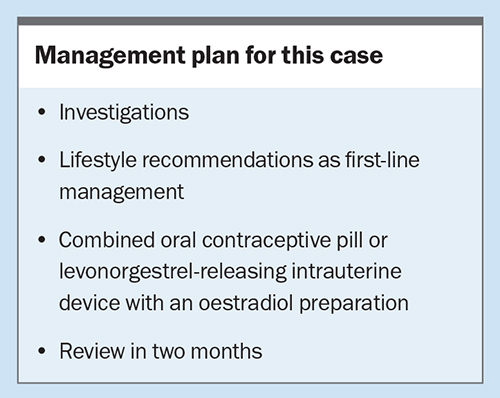
If all of Ms A’s investigation results are normal except for the bulky uterus found on the ultrasound and examination, determine the most appropriate treatments available. Ms A should be asked to diarise her symptoms and bleeding to assess improvement and be given a copy of her treatment plan, summarised in the Box.
Conclusion
Menopause treatment options vary with the phase at which a woman presents – in the perimenopause, the immediate postmenopause or some years later. Her symptom complex, past and family history and her own preferences will guide her treatment. Above all, it is important to tailor the therapy to meet each individual woman’s needs. ET
COMPETING INTERESTS: Dr Farrell has received consultation fees from Vifor Pharma and
Theramex; presented lectures for Vifor Pharma, Besins Healthcare and Theramex; is a Gynaecology Consultant to Medical Panels Victoria; and is Medical Director and Board Member for Jean Hailes for Women’s Health.
References
1. Harlow S, Gass M, Hall J, et al; STRAW 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Menopause 2012; 19: 387-395.
2. Hale GE, Hughes CL, Burger HG, Robertson DM, Fraser IS. Atypical estradiol secretion and ovulation patterns caused by luteal out-of-phase (LOOP) eventsunderlying irregular ovulatory menstrual cycles in the menopause transition. Menopause 2009; 16: 50-59.
3. Christin-Maitre S, Laroche E, Bricaire L. A new contraceptive pill containing 17B-oestradiol and nomegestrol acetate. Womens Health (Lond) 2013; 9: 13-23.