Infection in people with diabetes: what might be avoided?
Infection with bacterial, viral and fungal pathogens occurs more frequently in people with diabetes, and for some infections poorer outcomes may occur. Several opportunities exist, both directly and indirectly related to diabetes care, that may be useful for reducing infections in people with diabetes.
- Several different infections occur more frequently in people with diabetes and may have worse outcomes.
- Effective management of diabetes, including both acute and chronic glycaemia, may reduce risk of infections.
- Vaccination is a safe and effective way of preventing some infections, especially influenza and pneumococcal infections.
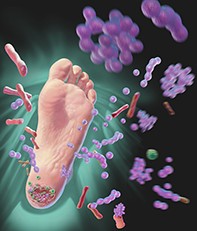
- Foot care and engaging podiatrists is important in preventing ulceration and infection in the diabetic foot.
About 6% of the Australian population self-report a diagnosis of diabetes mellitus. Proportionately, people who are older, of lower socioeconomic status or who are Aboriginal or Torres Strait Islander are more likely to have been diagnosed with diabetes.1,2 People with diabetes are more susceptible to many common infections, as well as some unusual and severe infections.3 Risk of infection-related hospitalisation among people with diabetes may be as high as 5% per year, which is double that among people without diabetes; and outcomes for people with diabetes and severe infections requiring hospitalisation are also worse.3-5
Mechanisms of increased susceptibility to infection in diabetes
Hyperglycaemia has acute and chronic effects on the immune system and predisposes people to other disease states (for example, neuropathy and impaired tissue perfusion from peripheral vascular disease) that may increase the risk of infections. Impairment of the innate immune system in people with diabetes includes reductions in polymorphonuclear (neutrophil) cell mobilisation, chemotaxis, phagocytic activity and superoxide burst.3,4,6,7 Such changes relate to both acute (especially blood sugar levels of greater than 12 mmol/L) and chronic hyperglycaemia, and some of the neutrophil dysfunction may quickly reverse with insulin therapy and restoration of euglycaemia.4 Cell-mediated immunity may be affected by hyperglycaemia, with reduced T-lymphocyte cell proliferation in patients with type 1 diabetes and HbA1c of greater than 8 mmol/L.4 Tight glycaemic control may help normalise these responses. Decreased levels of complement (C4) and increased background levels of the inflammatory cytokines tumour necrosis factor-alpha, interleukin-6 and interleukin-8 may lead to reduced responsiveness to stimulation.6 Antibodies may be susceptible to glycosylation, although the impact of this on their function is uncertain. Several comprehensive reviews of the effects of diabetes on immune system function have been published.4,6-8
When these immune system defects are considered in the context of comorbidities frequently seen in people with diabetes (especially type 2 diabetes), a synergistic increased risk for infection may occur. Additional factors involved may be vascular disease, neuropathy (sometimes with gastrointestinal tract dysfunction), glycosuria and increased use of health care services (and associated invasive procedures and devices). Specifically, in the foot, the triad of neuropathy, impaired vascular supply and deformity places the foot at higher risk of ulceration and subsequent infection.6,9
Infections and diabetes
Many infections occur more frequently in people with diabetes, and some infections are rarely encountered in people without diabetes (Figure 1).3-6 Remarkably, in a large Canadian cohort study, nearly half of the patient group with diabetes attended their primary care physician during a one-year period for management of infection, and 5% of patients were hospitalised for infections.3 Further, large studies conducted in Australia, the UK, the Netherlands and Denmark found similar increased rates of infections among people with diabetes, with type 1 diabetes conferring a greater relative risk of infections than type 2. Outcomes from both pneumonia and nonpulmonary infections may be worse, and increased risk of death was shown.4 Table 1 shows estimates of risk of some common infections and outcomes among people with diabetes.3,5,10-13
A relationship between glycaemic control and both risk of community-onset infection and perioperative adverse outcomes including infection has been shown.10,14,15 Better management of diabetes before hospitalisation is associated with shorter length of stay.14 Tight perioperative glucose control in elective surgery patients has had variable effects on overall outcomes including cardiovascular events but is associated with lower risks of perioperative infection (relative risk, 0.59), predominantly wound infection. Tight perioperative glucose control may reduce immediate perioperative mortality (relative risk, 0.69); however, it is associated with increased episodes of hypoglycaemia.15
What might be avoided: reducing risks of infection in people with diabetes
Prevention of many diabetes-related infections is possible through management of glycaemia, vaccination, screening for diabetes-associated infections and diabetes-specific podiatry care (Figure 2). Attending to patients’ background comorbidities and general health care is important. Table 2 presents a selection of resources for healthcare providers and patients.
General considerations
Several of the studies discussed and presented in Table 1 demonstrated a risk associated not only with having diabetes, but incrementally with increased glycaemia. Long-term glycaemic management in diabetes is proven to reduce the risk of most known complications, and reduced infection risk is likely to be a benefit. People with diabetes may have comorbid medical conditions or frailty and a requirement for supportive or residential accommodation. Attention to physical (including nutritional), medical and psychological components is the basis of holistic diabetes care. Where complexity of requirements exists, complex care planning including engagement of multidisciplinary and team care from community providers or health services may form an important component of patient management.
Notably, in some subsets of patients with diabetes and cardiac or renal disease, certain groups of drugs have apparent benefits beyond glycaemic control in reducing risk of cardiovascular and renal events. Among these are the sodium-glucose cotransporter-2 (SGLT-2) inhibitors (e.g. dapagliflozin, empagliflozin and ertugliflozin), whose use is becoming increasingly widespread due to these benefits. However, these drugs may be associated with increased urogenital bacterial and fungal infections, and possibly Fournier’s gangrene, owing to their mechanism of action.16,17 Remaining aware and vigilant to this slight increased risk when prescribing these agents allows their safe use, and risk of infection is not generally a barrier to patients undergoing therapy with this class of medication.
Vaccination
Vaccine responsiveness in people with diabetes is largely preserved and similar to that of age-matched controls for influenza, and large cohort studies have shown a reduction in hospitalisations, noninfectious health events (e.g. stroke), pneumonia and death in influenza-vaccinated people with diabetes.4,18,19 Efficacy of both the 13-valent conjugate and the 23-valent polysaccharide pneumococcal vaccines has been shown, with reduction in hospitalisations and proven invasive pneumococcal disease, particularly in elderly patients who are at increased risk of pneumococcal infection.20,21 Administration of both of these vaccines as scheduled in the Australian Immunisation Handbook is an important aspect of care for people diagnosed with diabetes, especially older people. The relative risk for shingles (herpes zoster) is 1.3 among people with diabetes, and people over 60 years of age should be considered for zoster vaccination.22 People with diabetes who plan travel can receive vaccinations determined by their travel destination, including live vaccines (for example Japanese encephalitis vaccine and yellow fever vaccine), and should carry details of their diabetes care when they travel. Additionally, patients should be advised to keep up to date with diphtheria, tetanus and pertussis vaccinations (especially if in contact with pregnant women and infants). Vaccinating all members of households of people with diabetes for influenza can further reduce risk of acquisition.
Elective surgery
People with diabetes who are undergoing elective surgery should have their diabetes management optimised in the lead up to the procedure, as this is associated with reduced lengths of stay and postoperative complications. In hospital, perioperative attention to hyperglycaemia may reduce cardiovascular and infection complications of surgical procedures.14,15 People with diabetes are more likely to be colonised with Staphylococcus aureus, including methicillin-resistant S. aureus, and carriage of this organism before surgery represents a risk factor for perioperative infection.4,23,24 Decolonisation techniques for S. aureus are well described and should be considered when patients are known or found to be colonised with this organism.24
Managing the foot
Superficial fungal infections and bacterial infection of the foot (cellulitis) occur more frequently in people with diabetes (Table 1). People with diabetes are at risk of ulceration due to neuropathy, ischaemia and deformity, with subsequent risk of infection (‘diabetic foot infection’).11 Consequences of diabetic foot infections can include amputations and death. Long-term optimal glycaemic management may reduce the risk of these complications, and several strategies to prevent ulceration of the feet in people with diabetes are described.11 Foot management should include regular scheduled podiatry assessment including advice on appropriate foot care and footwear. When foot infection is present, prompt assessment, grading the severity of the infection using validated tools, prescribing antibiotics according to predicted pathogens, and prompt referral for moderate to severe infections may help avoid progressive infection and amputations.25
Infections related to and interactive with diabetes
In people with diabetes, specific screening for hepatitis C and tuberculosis should be considered. Hepatitis C infection is associated with an increased risk of impaired fasting glucose levels and onset of type 2 diabetes. People diagnosed with type 2 diabetes should undergo screening for risk factors for carriage of hepatitis C virus, and if present, testing for this infection. Treatment and cure of hepatitis C infection reduces hepatic complications (which are otherwise amplified by the presence of diabetes) and contributes to diabetes management, as improved glucose tolerance may result.26 Patients should also be asked about risk factors for Mycobacterium tuberculosis infection (the most common being prior residence in a tuberculosis-endemic country for greater than three months). If risk factors are present, screening for latent disease with interferon-gamma release assays may be considered. Reactivation rates of latent tuberculosis are higher among patients with diabetes (relative risk, 1.6–2.6); however, in the Australian setting the absolute risk of active tuberculosis disease, especially for people born in Australia, remains negligible and screening may not be justified.9 See the Box for information about SARS-CoV-2 (COVID-19) infection in people with diabetes.27-29
Conclusion
Diabetes increases the risk of many infections as well as requirements for health care more generally. In addition to tight management of glycaemia, several other widely available and accessible strategies exist to reduce infections in people with diabetes, including vaccination, and specific attention to bacterial colonisations and glycaemic management in the perioperative period. Further, including regular podiatric care can avoid complications relating to neuropathy and vasculopathy in the foot. Resources, including several for patients and healthcare providers specific to the Australian context, are readily available. Strategies to prevent infection, and optimal management when infection does occur, are a priority in the routine care of people with diabetes. ET