Peer Reviewed
Feature Article Endocrinology and metabolism
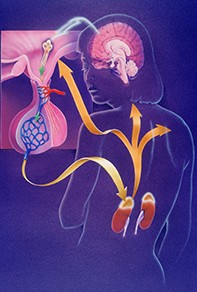
Addison’s disease: a diagnosis not to be missed
Abstract
Addison’s disease is a potentially life-threatening disorder caused by deficiencies of all adrenocortical hormones. A high index of suspicion is needed because the presentation is often nonspecific and can mimic other medical and psychiatric conditions. Prompt recognition and treatment is essential and life saving.
Key Points
- Addison’s disease should be suspected in patients presenting with hyperpigmentation of skin and oral mucosa, unexplained weight loss, persistent hyponatraemia or other autoimmune diseases associated with polyendocrinopathy syndrome.
- The initial test in patients with suspected Addison’s disease is the measurement of basal morning plasma cortisol and adrenocorticotrophic hormone (ACTH) levels. A basal morning plasma cortisol level of less than 100 mmol/L is diagnostic of adrenal insufficiency. Plasma ACTH levels are elevated in patients with Addison’s disease.
- The short Synacthen test should be performed if basal plasma cortisol levels are nondiagnostic.
- Treatment should not be delayed in patients with suspected adrenal crisis while awaiting diagnostic confirmation.
- Referral of the patient to an endocrinologist is essential in cases of equivocal diagnostic tests with high clinical suspicion of adrenal insufficiency and for long-term management of diagnosed Addison’s disease.
Picture credit: © Bob L. Shepherd/Science Source/Diomedia.com
Purchase the PDF version of this article
Already a subscriber? Login here.