Anabolic therapy: a new paradigm for osteoporosis management
Osteoporosis is a chronic condition that requires a whole-of-life approach to prevent fractures. Antiresorptive therapies such as bisphosphonates and denosumab are effective medications to improve bone density and reduce fracture risk. In patients at very high risk of fractures, anabolic agents are effective in promoting bone mass gain and providing more potent and rapid antifracture effects.
- Osteoporotic fractures are associated with significant morbidity and premature mortality.
- Antiresorptive medications such as bisphosphonates and denosumab are effective treatments for osteoporosis and significantly reduce fracture risk.
- Patients at very high risk of fracture include those with recent or recurrent fractures, very low T-scores, glucocorticoid use and high risk of falls.
- Anabolic therapies, such as teriparatide and romosozumab, stimulate bone formation. They result in significantly lower risk of fracture compared with antiresorptive treatments. These treatments are PBS-subsidised for use in people who experience fractures while on antiresorptive therapies.
- GPs play an integral role in identifying patients at very high risk of fracture who would benefit from specialist referral and initiation of anabolic treatments.
- Following a course of anabolic treatment, patients require subsequent treatment with an antiresorptive agent to consolidate gains in bone density and further reduce fracture risk.
Osteoporosis affects more than 1.2 million Australians.1 One fracture is estimated to occur every 3.4 minutes due to poor bone health, costing the Australian healthcare system in excess of $2 billion per year in direct costs including hospital stays, surgery, emergency assistance, rehabilitation and community care.2 Hip fractures alone account for 43% of direct costs, adding up to $962 million in total direct costs per year.3 More than 50% of postmenopausal women and 30% of older men will suffer at least one osteoporotic fracture during their lifetime. This can lead to chronic pain, decreased mobility and loss of independence, and affect quality of life. Fractures result in further fractures and are associated with premature mortality.4,5 This article discusses the use of anabolic therapies and key features of the patients at high risk of fracture in whom anabolic therapy is appropriate.
Patients at very high risk of fractures
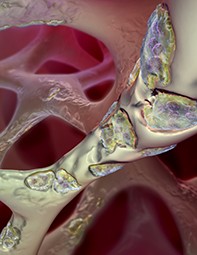
Some patients with osteoporosis have a critical degree of bone microstructural deterioration and are at very high risk of fractures. Identifying these patients may help guide the choice of drug treatment in osteoporosis. Certain clinical features can aid in identifying patients who are at very high risk of fractures. These include recent or multiple fractures, fractures while receiving osteoporosis therapy, long-term glucocorticoid therapy, low T-scores (≤−3.0 SD) and high risk of falls (Box). Fracture risk score calculators (such as the Garvan Institute’s bone fracture risk calculator or the Fracture Risk Assessment Tool [FRAX]) are available online and may also aid in identifying patients at high risk of fractures.6-8
Patients with recent or recurrent fractures, particularly hip and clinical vertebral fractures, are at higher risk of further fractures.5,9,10 This risk is particularly high within the first five years after the first fracture, and excess mortality, partly due to subsequent fractures, is observed up to 10 years after the initial fracture.11 Despite this, a significant proportion of people with fractures do not receive treatment for osteoporosis. The osteoporosis evidence–practice gap may be attributable to a number of factors including a perceived lack of urgency for treatment of a condition with preventative medications and poor patient awareness of osteoporosis and its impact on fracture risk and future health.12 Media reports of rare complications such as osteonecrosis of the jaw after prolonged antiresorptive therapies have also had negative impact on patient acceptability of and adherence with osteoporosis treatment.13 Consensus guidelines, such as the RACGP osteoporosis guidelines, aim to highlight these issues and provide clear, evidence-based recommendations to assist GPs and other healthcare providers in managing osteoporosis.14
Those who receive treatment for osteoporosis with potent antiresorptive agents, such as denosumab or bisphosphonates, have a relative risk reduction in vertebral fracture risk of 70%, seen over three years of treatment. However, the reduction of nonvertebral fracture risk is more modest, at 20 to 40%.15,16 Patients at high risk of fractures may need more potent and faster acting treatment to reduce their vertebral and nonvertebral fracture risk.
Antiresorptive therapy for osteoporosis
Bone loss in osteoporosis occurs due to an imbalance between bone resorption by osteoclasts and bone formation by osteoblasts. Antiresorptive medications inhibit osteoclast activity and viability, leading to reduced bone resorption. Bisphosphonates, including weekly oral alendronate or risedronate, and annual intravenous zoledronic acid are approved treatments for osteoporosis and significantly reduce the risk of minimal trauma fractures. The HORIZON Pivotal Fracture trial demonstrated the efficacy of once-yearly zoledronic acid in significantly improving bone mineral density (BMD) and reducing vertebral, nonvertebral and hip fractures in postmenopausal women by 70%, 25% and 41%, respectively, over three years of treatment.16 Denosumab is a fully humanised monoclonal antibody that binds to the receptor activator of the nuclear factor-kB ligand (RANKL); blocking this osteoclast activator impairs osteoclast formation, survival and function, and thereby inhibits bone resorption.17 The efficacy of denosumab for the treatment of osteoporosis was demonstrated in a large randomised controlled trial in which vertebral, nonvertebral and hip fractures were reduced by 68%, 28% and 40%, respectively, at 36 months.16 This benefit extends with treatment for up to 10 years, with sustained increases in BMD of 21.7% at the lumbar spine, 9.0% at the femoral neck and 2.7% at the distal radius from baseline, and sustained reduction in fracture risk.18
Anabolic therapy for osteoporosis
Anabolic therapy for osteoporosis increases BMD and reduces fracture risk by stimulating bone formation by osteoblasts. Patients at very high risk of osteoporotic fractures (Box) who have multiple or recurrent fractures despite antiresorptive therapy should be referred to a specialist or consultant physician for consideration of anabolic therapy. In Australia, two anabolic agents are currently available for the treatment of osteoporosis, teriparatide and romosozumab (Table).
Parathyroid hormone
Parathyroid hormone (PTH) stimulates both bone formation and resorption. Continuous infusion and persistently elevated levels of PTH, as seen in primary hyperparathyroidism, leads to bone loss. However, intermittent daily dosing of PTH agonists stimulates a net increase in bone formation, leading to increased bone strength.19
Teriparatide, a 1-34 PTH peptide, showed significant reduction in vertebral (65%) and nonvertebral (53%) fractures within a median treatment period of 19 months compared with placebo.20 Compared with a weekly oral bisphosphonate, there was a significant reduction in vertebral fracture risk of 56% as well as a trend towards reduced nonvertebral fracture incidence over a two-year period in postmenopausal women randomised to teriparatide.21 Teriparatide was approved by the TGA in 2003 and is currently subsidised by the PBS for patients with severe osteoporosis (T-score ≤−3.0 SD) with two or more minimal trauma fractures and at least one new symptomatic fracture while using antiresorptive therapy.22 Teriparatide is also TGA-approved for the treatment of osteoporosis associated with sustained systemic glucocorticoid therapy.
Teriparatide is available in a multidose, prefilled pen and is administered as a daily subcutaneous injection of 20 mcg for 18 months. Patients need initial education in self-administering the dose and a specialist or a consultant physician must initiate treatment; GPs can provide subsequent scripts.
The main adverse events of teriparatide are nausea, dizziness, headaches and mild hypercalcaemia. These side effects may be less problematic if teriparatide is taken in the evening. Preclinical rodent models suggested a potential association between teriparatide use and osteosarcoma with prolonged continuous exposure at high doses. Therefore, the maximum lifetime duration of PBS-subsidised teriparatide therapy is 18 months (TGA approval for 24 months). An additional six months of teriparatide therapy can be considered for patients with severe osteoporosis who remain at high risk of fractures after 18 months; however, this will need to be self-funded by the patient.
Reassuringly, post-marketing surveillance studies over 15 years have shown no increase in teriparatide-related osteosarcoma and, therefore, this is no longer a concern in humans.23,24 However, the risk to patients with known bone metastases or bone malignancy has not been established. Patients with an unexplained elevated alkaline phosphatase (ALP) level should be evaluated for Paget’s disease before commencing teriparatide use. Teriparatide is contraindicated in those who have previously received radiotherapy to the skeleton and should also be used with caution in those with a history of kidney stones due to the risk of hypercalciuria. However, the increase in urinary calcium excretion is typically negligible and patients do not require routine urinary calcium monitoring.25
Regardless of treatment duration, teriparatide must be followed with antiresorptive therapy such as bisphosphonate or denosumab to maintain the gains in bone density achieved by this anabolic agent.
Abaloparatide is an analogue of PTH-related protein (1-34) that acts selectively on the PTH receptor to stimulate bone formation. Like teriparatide, it is administered as a daily injection and reduces vertebral and nonvertebral fracture risk. However, abaloparatide is not currently available in Australia.26
Romosozumab
Sclerostin is a signalling factor produced by the sclerostin gene (SOST) and secreted by osteocytes that inhibits bone formation by downregulating osteoblast development and activity. Therapeutic implications of inhibiting sclerostin came to light in the description of a rare genetic condition, sclerosteosis, seen in the Dutch Afrikaans community in South Africa, and characterised by high bone mass, protection from fracture and pathological bone overgrowth. The identification of loss-of-function variants of SOST in this condition led to the development of therapeutic agents targeting sclerostin production.27
Romosozumab is a monoclonal antibody that inhibits sclerostin, leading to a dual action of increased bone formation and reduced bone resorption. It is administered as a monthly subcutaneous dose of 210 mg, given in two subcutaneous injections of 105 mg each for 12 months. It can be administered subcutaneously in the abdomen, thigh or upper arm. Dose adjustment is not required in patients with renal impairment, although the risk of hypocalcaemia is higher in those with severe renal impairment (eGFR <30 mL/min/1.73m2). Before starting a patient on romosozumab, it is important to ensure their serum vitamin D level is above 50 nmol/L and daily calcium intake is at least 1000 mg, as hypocalcaemia can occur, particularly after the initial dose.
The pivotal FRAME study showed a 73% reduction in vertebral fracture risk, 36% reduction in clinical fracture risk and 25% reduction in nonvertebral fracture risk within the first 12 months of treatment in postmenopausal women receiving romosozumab compared with placebo.28 Significant increases in BMD were attributed to increased bone formation and reduced bone resorption. The predominant adverse events reported were injection site reactions, which were mostly mild in severity.
In a study comparing romosozumab with alendronate in postmenopausal women with osteoporosis and a fragility fracture, a numeric imbalance was observed in the incidence of serious cardiovascular adverse events, including coronary ischaemia and cerebrovascular events (2.5% in the romosozumab group vs 1.9% in the alendronate group). The significance of this finding is unclear; it may suggest that bisphosphonates can protect against cardiovascular disease.29 Conversely, there is biological plausibility for a link between sclerostin inhibition and vascular changes due to the expression of sclerostin in vascular smooth muscle. Until the risk of cardiovascular adverse events in patients on romosozumab is clarified, this agent should be used with caution in patients with a recent history of ischaemic heart disease or stroke and avoided in patients who have had a myocardial infarct or stroke in the preceding year.
As of 1 April 2021, romosozumab has been available in Australia. The indication for PBS-subsidised therapy is the same as for teriparatide (Table). Patients who have received teriparatide previously are not eligible to receive PBS-subsidised treatment with romosozumab; however, if they develop severe intolerance to teriparatide that necessitates permanent withdrawal from treatment within the first six months, they may be eligible for PBS-subsidised treatment with romosozumab. Similarly, patients who have received romosozumab previously are not eligible to receive PBS-subsidised treatment with teriparatide, unless they develop severe intolerance to romosozumab within the first six months of treatment that necessitates permanent withdrawal from treatment.
Sequential and combination therapy
Osteoporosis is a progressive, chronic condition and therapeutic strategies that provide long-term protection from fracture should be considered. GPs play an important role in identifying patients with fracture requiring osteoporosis therapies, and those at very high risk of fracture who should be referred for specialist opinion for anabolic treatment.
Currently, anabolic therapies are PBS-subsidised for patients who experience fractures while receiving antiresorptive therapy. Interestingly, anabolic treatments have greater gains in bone density when used before antiresorptive treatments. Comparison studies, such as the VERO study, comparing teriparatide with risedronate, or the ARCH study comparing romosozumab with alendronate, showed greater increases in BMD and more rapid reduction in fracture risk in patients on the anabolic therapies.21,29
Prior antiresorptive treatment may blunt BMD responses to anabolic therapy. Prior treatment with bisphosphonate therapy in patients receiving teriparatide was associated with loss of hip BMD in the first year after the switch.30 However, a study in which patient taking alendronate were transitioned to romosozumab showed a continued increase in hip and spine BMD, suggesting romosozumab may be the anabolic agent of choice for patients on bisphosphonates who have severe hip osteoporosis or previous hip fractures.31
Particular caution should be taken when switching patients from denosumab to another therapeutic agent. Although denosumab therapy reduces the risk of vertebral fractures, the risk returns to the level before treatment once therapy is stopped.32 Discontinuation of denosumab can lead to rapid bone loss, which may be associated with the development of spontaneous vertebral fractures. Transitioning from denosumab to a bisphosphonate may attenuate this bone loss; however, the optimal regimen following denosumab discontinuation remains unclear. In a randomised controlled trial, women switched from denosumab to teriparatide experienced accelerated bone loss within six months, particularly at the hip and distal radius.33 Therefore, switching from denosumab to teriparatide should be undertaken with caution, and clinicians may consider continuing denosumab while commencing teriparatide in patients requiring an osteoanabolic agent.
There are minimal data to guide transition from denosumab to romosozumab. Post-hoc analysis of a phase 2 trial showed that transitioning to romosozumab after 12 months of denosumab improved lumbar spine BMD and maintained total hip BMD.34
Treatment with anabolic therapies should be followed by antiresorptive treatment. Fracture risk remained significantly lower in patients who received antiresorptive treatment with bisphosphonate or denosumab after initial anabolic therapy with PTH-analogues or romosozumab. After teriparatide therapy, sequential treatment with denosumab was more effective than a bisphosphonate in increasing spine and total hip BMD.33 Both denosumab and alendronate have been shown to maintain increases in BMD and reduce fracture risk when used sequentially after romosozumab.28,29
Combination therapy with anabolic and antiresorptive therapy has been explored. The combination of bisphosphonates and teriparatide do not appear to provide significant benefit over monotherapy.35 Pivotal trials exploring the efficacy of combination therapy with teriparatide and denosumab have shown a significant improvement in BMD and fracture risk in patients who have not received prior treatment with an antiresorptive agent.36,37 This combination, however, is currently not TGA approved. There are no data examining the effects of combined treatment with teriparatide and denosumab on fracture risk reduction or long-term safety.
Conclusion
Osteoporosis is a chronic, progressive condition and requires a whole-of-life approach to treatment. Anabolic therapies, such as teriparatide and romosozumab, are indicated in patients at high risk of fracture. They are superior to antiresorptive therapies in promoting greater increases in bone density and more rapid and effective reductions in fracture risk. Although the benefits of anabolic therapy are maximal when used as initial therapy, they are currently PBS-subsidised for patients who fracture while receiving antiresorptive therapy and those who remain at high risk of fractures. After treatment with an anabolic agent, patients should receive antiresorptive therapy to maintain skeletal benefits. GPs play an important role in bridging the osteoporosis evidence–practice gap and identifying patients who would benefit from pharmacological management of osteoporosis, particularly those at very high risk of fractures who would benefit from specialist referral for anabolic therapy. ET
COMPETING INTERESTS: None.