Acute adrenal insufficiency: optimising care
Adrenal crises are severe, life-threatening episodes of adrenal insufficiency. Preventing and managing adrenal crises is complex and current strategies have not been successful in achieving a reduction in the incidence of episodes. Treatment with intravenous hydrocortisone is life saving and should be given without delay to patients displaying signs of acute adrenal insufficiency and adrenal crises.
- An adrenal crisis is an acute episode of adrenal insufficiency that is characterised by hypotension and other symptoms and signs, including reduced consciousness, acute abdominal symptoms and electrolyte abnormalities.
- Treatment with intravenous hydrocortisone should be given urgently and never withheld because of concerns about the side effects of glucocorticoid exposure.
- All patients with adrenal insufficiency should carry a steroid identification card, belong to the MedicAlert Foundation (or equivalent), have adequate supplies of oral replacement therapy and have their own hydrocortisone intramuscular injection vial and needles.
- At each review, patients should be reminded about the importance of adrenal crisis prevention and the steps involved in glucocorticoid stress dosing and be assessed for competency with intramuscular self-injection of hydrocortisone. For patients unwilling or unable to inject intramuscularly, subcutaneous injection before clinic presentation should help avoid deterioration and severe shock.
An adrenal crisis may be the first presentation of a patient with undiagnosed adrenal insufficiency. However, adrenal crises usually occur in people with known hypoadrenalism, providing an opportunity to prevent these episodes. This article outlines the pathophysiology and methods of management and prevention of adrenal crises in patients with adrenal insufficiency.
Adrenal crises occur at a rate of five to 10 per 100 patient years in people with adrenal insufficiency and have an estimated mortality rate of 0.5 per 100 patient years.1 They arise when the requirement for cortisol is greater than the amount available in the circulation, usually in situations of physiological stress such as infection, gastroenteritis, injury or a surgical operation.2,3 The diagnostic hallmark of an adrenal crisis is hypotension due to hypovolaemic shock. Other symptoms and signs that may also be present include hyponatraemia, hyperkalaemia, nausea and vomiting, abdominal pain and confusion.2,3
Glucocorticoid dose escalation (stress dosing), which comprises an increased oral replacement dose and/or parenteral hydrocortisone (if the oral dose cannot be taken or has not been effective) is used to increase the level of circulating cortisol and to prevent the development of an adrenal crisis.3 Empowerment of patients to confidently self-manage stress dosing during intercurrent illness is essential, but evidence indicates that patient education is not sufficient to prevent many adrenal crises.1
The persistent occurrence of these events in treated adrenal insufficiency is of great concern to patients and their families and requires increased resolve on the part of healthcare professionals to assist patients to manage episodes of illness and to intervene with intravenous hydrocortisone promptly when patients are acutely unwell.
Definition and diagnosis
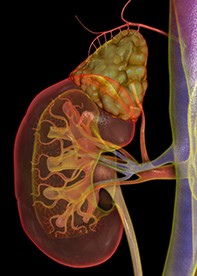
There is no generally agreed definition of an adrenal crisis and this can lead to confusion around the diagnosis and a delay in life-saving treatment.2 To address these problems, we propose a definition that includes objectively measurable criteria. It states that an adrenal crisis is: ‘An acute deterioration in health that is associated with absolute (systolic blood pressure [BP] less than 100 mmHg) or relative (systolic BP 20 mmHg lower than the patient’s usual BP) hypotension, the features of which resolve following parenteral glucocorticoid administration (demonstrated by a marked resolution of hypotension within one hour and improvement of clinical symptoms over two hours)’.3 The Figure illustrates the physiological processes involved in the adrenal insufficiency syndrome.
Frequent concomitant features of an adrenal crisis include acute abdominal symptoms, delirium/obtundation, hyponatraemia, hyperkalaemia, hypoglycaemia and pyrexia.3 Although this definition applies to adults, older children and adolescents, in young children with adrenal insufficiency hypotension may be more difficult to identify and other features may be more prominent. Therefore, we have defined an adrenal crisis in young children as: ‘an acute deterioration in health that is associated with acute haemodynamic disturbance (hypotension or sinus tachycardia relative to age-related normal levels) or a marked abnormality in one or more electrolytes (hyponatraemia, hyperkalaemia) or hypoglycaemia that is not attributable to another illness, the features of which show significant resolution following parenteral glucocorticoid administration’.4
As in the other age groups, there are a number of symptoms and signs that may be present in a young child who is experiencing an adrenal crisis. These include acute abdominal symptoms, altered levels of consciousness/obtundation, nausea and vomiting, abdominal pain, poor feeding (in infants) and pyrexia.4
In all age groups, consideration of other illnesses and potential causes for shock can improve the specificity of the adrenal crisis diagnosis. Other potential illnesses that may mimic an adrenal crisis include any cause of shock, acute abdomen or septicaemia. A poor response to parenteral glucocorticoid should prompt re-evaluation of the patient for other complicating illnesses.
It is important to note that some of the symptoms and signs that are typical of an adrenal crisis, for example nausea and vomiting, may also be present in patients with adrenal insufficiency who are unwell but not hypotensive and, therefore, would not be categorised as having an adrenal crisis. We recommend that these patients be classified as having symptomatic adrenal insufficiency or a pre-crisis or incipient crisis.3 They may need treatment with intravenous hydrocortisone and fluids to relieve their symptoms and to avoid progression to an adrenal crisis.
Prevention
In patients with diagnosed adrenal insufficiency, anticipatory or contemporaneous provision of additional glucocorticoid to mimic the stress response to illness, injury or surgery helps to prevent an adrenal crisis or shorten the duration of symptoms.5 All patients with adrenal insufficiency should be educated so that they can identify situations that require stress doses of glucocorticoid and can confidently manage dose escalation correctly during the course of an intercurrent illness.
Oral stress dosing involves either doubling or tripling the usual replacement dose during physiological stress (e.g. infection or injury). Generally, acute illnesses associated with fever can be categorised according to severity, with temperature below or above 38.5°C requiring either double the oral glucocorticoid dose for two days or triple the dose for three days.6 For many patients taking hydrocortisone a dose of one 20 mg tablet three times a day will be a practical way of remembering their treatment in these circumstances.
Patients should also be made aware of the importance of continuing their glucocorticoid replacement and be cognisant of the dangers of cessation of therapy or missed doses, as this can also lead to the development of an adrenal crisis. In addition, patients with adrenal insufficiency requiring a surgical procedure should discuss the need for glucocorticoid cover with their endocrinologist and surgeon.2,3,7 General recommendations for glucocorticoid cover according to the level of surgical intervention and other specific situations are shown in the Table.
Parenteral glucocorticoids
In situations where the patient’s oral glucocorticoid replacement dose cannot be taken or may not be absorbed (e.g. where there is vomiting or diarrhoea), parenteral hydrocortisone (typically 100 mg intramuscularly in adults) is recommended.2,3 Patients and their family members should be supported to achieve confidence and competency in the method of intramuscular injection of hydrocortisone and be provided with vials, needles and syringes. After self-injection, patients should be encouraged to attend hospital promptly, as should those patients who are unable to use parenteral hydrocortisone. It should be remembered that the plasma disappearance half-life of hydrocortisone is approximately 90 minutes, although its beneficial effects in tissues can be expected to last six to 12 hours.
Reluctance to administer an intramuscular injection is not uncommon among patients and their family members, and this may contribute to delays in proper preventive treatment in some patients. For this reason, hydrocortisone injected via the subcutaneous route has been suggested as an alternative.3,8,9 This approach is supported by evidence of the equivalent absorption of hydrocortisone by subcutaneous and intramuscular injection in patients who are not obese and not in active shock.8 Rectal hydrocortisone may be a preferable option for some patients, providing diarrhoea is not present.3 There is no requirement to increase fludrocortisone dose in acutely unwell patients with adrenal insufficiency because hydrocortisone in doses exceeding 50 mg per day provides sufficient replacement mineralocorticoid.
The potential for delay in access to definitive care (intravenous hydrocortisone) and the risk that this imposes is such that, when oral dose escalation has been ineffective or cannot be used, patients should be encouraged to self-inject before medical attendance. Patients need instruction on self-injection. Intramuscular injection is recommended by the manufacturer of hydrocortisone for injection, although subcutaneous injection also has suitable pharmacokinetics and is likely to be considerably safer than nonadministration in emergencies where intramuscular rather than subcutaneous self-injection is a barrier to use of parenteral hydrocortisone. Advice is also available via the Australian Addison’s Disease Association website (https://addisons.org.au).
Patients should also be advised to seek medical attention promptly when unwell, carry a steroid dependency card and have a membership of the MedicAlert Foundation (or equivalent) to enable identification of their adrenal insufficiency status in circumstances where they may be unable to communicate. Unfortunately, although this has not been documented in Australia, anecdotal evidence suggests that only a proportion of patients use these methods of identification regularly.
Precipitants
A range of factors may act as precipitants of an adrenal crisis.1-3 Infection, particularly gastroenteritis, is a frequently cited cause.1-3 This is especially dangerous in adrenal insufficiency, as vomiting and diarrhoea can impair the absorption of oral medication and may exacerbate dehydration. Other infections, especially bacterial infections including urinary tract infections and pneumonia, can precipitate an adrenal crisis.1,10,11 This appears to be more common in older patients, possibly due to increased susceptibility to bacterial infections in older age groups.11 By comparison, viral infections predominate in children with adrenal crises.4,12 Failure to take the recommended glucocorticoid replacement may also precipitate an adrenal crisis.
Other exposures, such as emotional stress and strenuous exercise, have been identified by some patients as adrenal crisis precipitants.1 Although cortisol secretion physiologically increases with both emotional upset and exercise, a study of short-term exercise in patients with Addison’s disease did not show any benefit of supplemental glucocorticoid administration.13 The potential benefit of stress dosing glucocorticoids for emotional stress has not been systematically studied. In some circumstances it could be potentially deleterious due to excessive central nervous system arousal. Recently, adrenal crises have been reported in association with acute phase reactions following vaccinations and the infusion of zoledronic acid to treat osteoporosis.14,15 They may also arise following autoimmune injury to the pituitary or adrenal glands as a result of treatment with immune checkpoint inhibitors for malignant disease.16,17 In a proportion of adrenal crisis cases (7% in one study) there is no obvious precipitant.1
Problems accessing appropriate health care, many of which are preventable, may also lead to an adrenal crisis. Delays in hydrocortisone administration, which may be deliberate or inadvertent, have resulted in an adrenal crisis in some patients.3,18 These may be due to the mistaken belief on the part of health professionals that the ill effects of glucocorticoids are greater than the risk of nonadministration of hydrocortisone to an ill patient with adrenal insufficiency.2,3 Difficulties accessing health services (ambulance and medical care) may also lead to crucial delays in the administration of hydrocortisone.5 In some patients, however, an adrenal crisis can evolve so rapidly that there is only a minimal opportunity to intervene before the onset of severe symptoms.2
Nonadherence to steroid replacement therapy is also a risk factor for an adrenal crisis. Patients with adrenal insufficiency should be aware of their need for ongoing glucocorticoid replacement and be warned of the dangers of omission of doses or cessation of therapy. This also applies to patients on long-term steroid therapy for other illnesses where the daily dose is above the replacement dose (3 to 5 mg prednisolone or equivalent per day).
Risk factors
All patients with adrenal insufficiency are at risk of an adrenal crisis, although patients with primary adrenal insufficiency are at a greater risk than those with secondary adrenal insufficiency, owing to the possibility of residual cortisol secretion in some patients with secondary adrenal insufficiency.3 Some patients are vulnerable to adrenal crises and have multiple episodes, whereas some never experience an adrenal crisis event. Patients with comorbid endocrine disorders (e.g. type 1 diabetes mellitus) appear to be at greater risk of adrenal crises than patients with primary adrenal insufficiency alone.3,19 The introduction of thyroid hormone replacement therapy in a patient with hypothyroidism who has undiagnosed adrenal insufficiency may initiate an adrenal crisis.
The use of glucocorticoids to treat a range of inflammatory and some malignant diseases means that adrenal insufficiency due to hypothalamic-pituitary-adrenal axis suppression is the most common form of adrenal insufficiency in the population. Although these patients may be at risk of an adrenal crisis, it is thought to be an uncommon occurrence.7 Nevertheless, these patients should be educated about the risks of intercurrent illness and surgery and be made aware of the need to avoid sudden cessation of glucocorticoid therapy.3
Management
An adrenal crisis is a medical emergency requiring urgent parenteral hydrocortisone and fluid resuscitation. In the emergency setting, attribution of symptoms and signs to an adrenal crisis depends on establishing either a pre-existing diagnosis of adrenal insufficiency or the clinical suspicion of this disorder. It is noteworthy that a substantial proportion of patients suffering an adrenal crisis have previously undiagnosed adrenal insufficiency and many have a history of typical symptoms that have been attributed to other disorders.20
Patients may have underlying primary adrenal insufficiency or Addison’s disease (often due to autoimmunity); secondary adrenal insufficiency, usually following pituitary tumours or their treatment; and tertiary adrenal insufficiency, resulting from disease of the hypothalamus (frequently included in the secondary category). Symptoms and signs of underlying primary adrenal insufficiency include hyperpigmentation, nausea and vomiting, anorexia, weight loss, fatigue, postural dizziness and syncope.3,6 The clinical presentation of secondary adrenal insufficiency is similar, although there is no hyperpigmentation.
Most patients suffering an adrenal crisis need hospitalisation and some may require admission to a high-dependency unit or intensive care unit. Emergency treatment involves the urgent administration of hydrocortisone and fluids. In adults, hydrocortisone is given as 100 mg intravenous bolus followed by 200 mg every 24 hours given as a continuous infusion or frequent intravenous (or intramuscular) boluses (50 mg) every six hours, with subsequent doses tailored to the clinical response.3 Where the diagnosis of adrenal insufficiency is suspected but not certain, blood should be taken for measurement of serum cortisol (and preferably also plasma adrenocorticotrophic hormone [ACTH]) before treatment. However, it is essential that hydrocortisone be given promptly and not withheld while waiting for tests, such as the short ACTH stimulation test.
In adults, intravenous fluids are generally given as normal saline 1000 mL within the first hour, with further crystalloid fluid being administered according to standard resuscitation guidelines and taking into account the patient’s circulatory status, body size and relevant comorbidities.3 Fluid should be given with particular caution in patients with treated diabetes insipidus, as excessive fluids may lead to hyponatraemia.3 Investigations and treatment of any underlying illness that may have precipitated the adrenal crisis and other comorbidities should be undertaken. In situations where there is no improvement after hydrocortisone and intravenous fluids, other causes of hypotension (e.g. sepsis, myocardial infarction or occult haemorrhage) should be sought.
After successful management of the adrenal crisis, stress doses of glucocorticoid should be tapered (typically over a few days) to the usual maintenance dose. Increasing the ongoing glucocorticoid maintenance dose to avoid a future adrenal crisis is not recommended unless the maintenance dose is below that recommended (e.g. hydrocortisone 15 to 25 mg per day or prednisolone 3 to 5 mg per day) as arbitrary increases in glucocorticoid dosing may induce Cushing’s syndrome or subtle effects of glucocorticoid excess such as centripetal weight gain or reduced bone density. Following the episode, it is recommended that the patient and their clinician assess the precipitants of the adrenal crisis, review any risk factors, reiterate the steps for prevention and re-evaluate the patient’s competency in parenteral glucocorticoid administration.
Conclusion
Preventing and managing adrenal crises is complex and current strategies have not been successful in achieving a reduction in the incidence of these episodes. Patient education, while necessary, is not sufficient for this purpose as adrenal crises continue to occur among educated patients. Nevertheless, all patients need to be educated and empowered to confidently implement dose escalation during physiological stress, such as an intercurrent infection. In situations where stress dosing has been ineffective or cannot be tolerated, self-administered intramuscular injection of hydrocortisone before attendance at a health service is essential. An adrenal crisis is a medical emergency and immediate attention is required for any patient with adrenal insufficiency who becomes acutely unwell. Importantly, hydrocortisone should be given urgently and not be withheld due to misplaced concerns about glucocorticoid exposure. ET